What Is Spinal Stenosis? Can It Cause Complications from Nerve Compression?
how we can help
An Overview
Spinal stenosis is a condition that falls under the broader category of nerve compression syndromes, where nerves are squeezed or compacted, often resulting in pain, numbness, and muscle weakness. This condition can arise from repetitive injuries, accidents, and certain medical conditions, affecting various peripheral nerves in the torso, limbs, and extremities.
The spine of a typical human being consists of 33 vertebrae bones that are stacked one on top of the other. These vertebrae have small “shock absorbers” called discs between them and have a spinal cord and millions of nerves running through a passageway from the low back all the way to the brain. If a “crimp” occurs in this cord because of age, injury or disease, causing a narrowing of the spinal canal, bodily movement becomes at best painful and at worst dramatically impeded.
The medical term for an abnormal narrowing or constriction of the diameter of a bodily passage or orifice is “stenosis.” When the passageway or “canal” containing the spinal cord and nerve roots is restricted or narrowed, this condition is called spinal stenosis. For millions of people, spinal stenosis is a chronically painful experience that seems almost unbearable.
Spinal stenosis is often discussed in the context of musculoskeletal and skin diseases by authoritative health organizations, highlighting its relevance within broader discussions of musculoskeletal disorders.
Spinal stenosis can be congenital, which means it is present at birth, or it can be acquired. This latter type of stenosis generally affects people 60 or more years of age.
One of the symptoms of this condition is nerve compression syndrome (link to blog article). This occurs when a nerve is squeezed or compacted, and it typically occurs at a specific location. Nerves in the torso, limbs, and extremities may be affected. This can lead to persistent pain in the butt region, weakness in the legs, limping, lack of feeling in the extremities, numbness in the fingers or toes or loss of bladder or bowel control. Often, patients have difficulty walking even relatively short distances because of leg symptoms of pain or weakness.
In a report from the National Institute of Health, the agency notes that spinal stenosis is a condition in which the nerve roots are compressed by a number of pathologic factors, leading to symptoms such as pain, numbness, and weakness. The upper neck (cervical) and lower back (lumbar) areas are most frequently affected, although the middle spine area (thoracic) also can be compressed, usually by a disc herniation.
The research from the NIH notes that three different anatomic sites within the canal can be affected by spinal stenosis. First, the central canal, which houses the spinal cord, can be narrowed leading to compression of neural elements and reduction of blood supply to the spinal cord in the cervical and the lumbar area. Secondly, the neural foraminal (often the C5 and C6 discs), which are openings through which the nerve roots exit the spinal cord, can be compressed because of disk herniation, excessive growth of the tissue of the facet joints and ligaments, or unstable slippage of a vertebra. Lastly, the lateral recess in the lumbar spine can be compressed from a tissue growth in the facet joint.
Table of Contents
Symptoms
Diagnosing
Treatments
Patients Ask:
What are the causes of spinal stenosis?
Texas Back Institute Responds: A variety of factors can cause spinal stenosis. Disc herniation or bulging can cause narrowing of the canal. Facet joints, which are on the sides of the canal, can also contribute to this condition. As we get older, the wear and tear on these facet joints can lead to what are called bone spurs or cysts which can cause this compression of the nerves. Finally, on the back of the spinal canal, some patients can experience abnormal growth of ligaments which can cause spinal stenosis.
Conditions like rheumatoid arthritis can also contribute to nerve compression syndrome.
(Insert photo or graphic of an older person who appears to be in pain, perhaps holding his/her back)
What Are the Symptoms of Spinal Stenosis?
Spine specialists like those at Texas Back Institute are well-trained in the detection of the symptoms of spinal stenosis. This can be tricky, because these “clues” will vary, depending on where the stenosis is occurring in the spine.
Patients who have stenosis in the neck or cervical region of the spine can develop shooting pain in their arms. They can also experience tingling or numbness in the arms. One of the more concerning symptoms of spinal stenosis in the neck area is called cervical myelopathy. With this condition, patients will develop clumsiness with their hands or when walking and they can also have headache symptoms. Of course, treating headaches or migraines is much different from treating cervical myelopathy, so it is imperative that a trained neurosurgeon is consulted for neck related symptoms.
In the thoracic or mid back region, spinal stenosis will be affecting the spinal cord itself and this will result in mid back pain. It can also cause leg problems such as numbness, muscle weakness, or weakness in the legs.
With spinal stenosis in the low back area, the symptoms can include shooting pains down the leg, low back pain, numbness, tingling or muscle weakness in the legs. An urgent symptom of low back spinal stenosis is the loss of bowel and bladder control. If this occurs, immediate medical attention is required.
Patients Ask:
What is it about spinal stenosis that causes the numbness and tingling in the body’s extremities - the hands, fingers, feet and toes?
Texas Back Institute Responds: With spinal stenosis, the space around the spinal cord becomes too narrow and this irritates the cord and/or the nerves that come off it. This can lead to tingling and numbness in the extremities of the body.
What About Headaches: “I have frequent headaches and periodic migraine headaches for which I have taken injections. Could cervical myelopathy be causing these headaches and how can I find out for sure?”
Texas Back Institute Responds: Severe headaches can be caused by a variety of factors, including spinal stenosis in the cervical or neck area. Only a neurosurgeon or spine specialist, using state-of-the-art diagnostic equipment, can help a patient understand and properly treat this condition.
Why Are L4 - L5 Vertebrae So Problematical for Lumbar Spinal Stenosis?
Depending on where they are located in the “spine stack,” vertebrae provide different degrees of load bearing and flexibility for the spine. A combination of evolution and patterns of wear and tear (due to the work and play that humans undertake) on the body have not been kind to the lumbar area of the spine, especially the L4 and L5 vertebrae.
This spinal segment consists of the two lowest vertebrae in the lumbar spine. It provides motion in many directions and supports the upper torso. The L4 and L5 undergo heavy impact with day-to-day motions and are highly flexible. This makes them particularly susceptible to injury and chronic conditions, including spinal stenosis. The L4-L5 vertebrae can affect the peripheral nerve, leading to symptoms like pain and numbness.
Spinal stenosis most commonly occurs in the lumbar spine, followed by the cervical spine. Lumbar spinal stenosis is usually caused by age-related spinal degeneration which can cause several changes in the spine that trigger stenosis. These include:
- Wear and tear on the facet joints of the spine (osteoarthritis)
- Bone spurs
- Bulging or herniated disks
- Thickened spinal ligaments
There are several symptoms of L4 – L5 that are troubling. These are:
- Debilitating pain in the lower back and leg
- Sexual dysfunction
- Constant pain, numbness, and/or tingling in the legs while standing
- Difficulty or inability to perform upright activities
- Bladder or bowel incontinence
- Severe weakness in both legs
- Numbness in the genital and inner thigh area
- Foot drop, where it is difficult or impossible to point the ankle and toes upward. This causes the foot to slap onto the ground while walking, with the leg dragging in front of the foot. Foot drops can also throw off balance.

Patients Ask:
Is spinal stenosis of the L4 and L5 treated differently than the cervical and thoracic areas?
Texas Back Institute Responds: All spinal stenosis treatments follow the same protocol, starting with a conservative, non-surgical approach and if this is not successful, surgery is discussed. See below.
How to Diagnose Nerve Compression from Spinal Stenosis
One of the critical considerations in the diagnosis of spinal stenosis involves understanding the problem. The spine specialists at Texas Back Institute begin the process with a diagnostic workup.
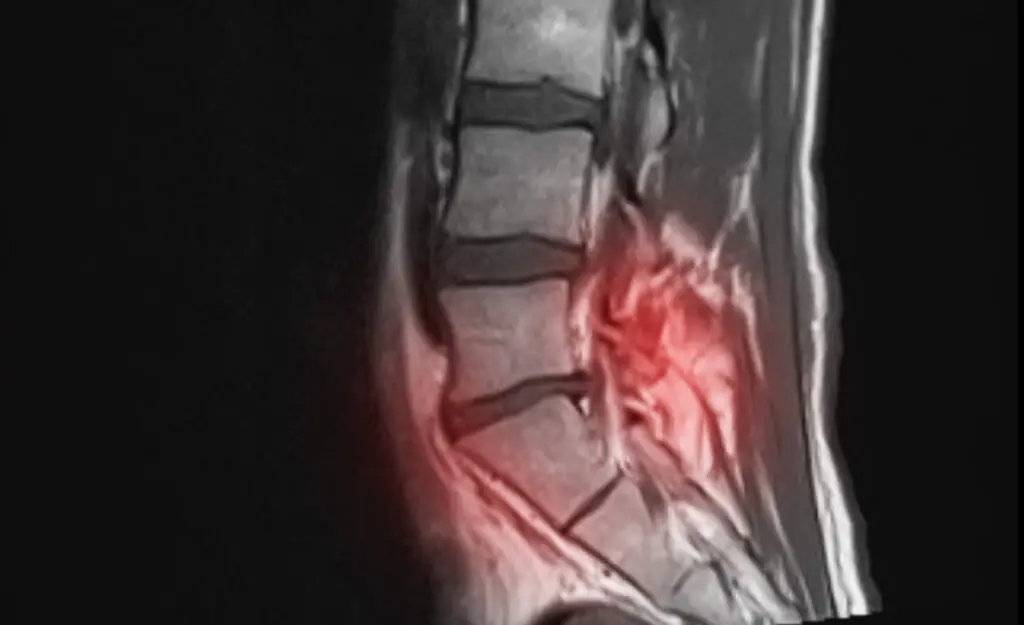
The optimum diagnostic test for this condition is an MRI (magnetic resonance imaging) scan. This is a medical imaging technique that is used to give physicians pictures of the spine and the physiological processes inside the body. These MRI scanners use powerful magnetic fields, magnetic field gradients, and radio waves to generate images of the organs in the body.
If an MRI is not possible, spine specialists can order a CT (computed tomography) myelogram scan. This diagnostic tool is a radiographic examination that uses a contrast medium to detect pathology of the spinal cord, including the location of a spinal cord injury, cysts, and tumors.
If the spine specialist at Texas Back determines a patient has nerve damage, electromyography (EMG) may be needed. An EMG measures muscle response or electrical activity in response to a nerve’s stimulation of the muscle. This test is used to help detect neuromuscular abnormalities by measuring the effectiveness of a patient’s nerves to conduct signals.
Patients Ask:
Are diagnostic procedures such as MRIs, CT myelogram scans or x-rays safe and effective for patients?
Texas Back Institute Responds: CT scans, MRIs and X-rays are all diagnostic tools that allow doctors to see the internal structures of the body. They create images using various forms of electromagnetic energy. When used by trained technicians, these tools are safe. However, they are somewhat different in their accessibility, resolution and the type of energy they use for imaging.
An X-ray is the fastest and most accessible form of imaging and this exam only takes a few minutes to complete. However, an x-ray will not show subtle bone injuries, soft tissue injuries or inflammation.
An MRI uses a powerful magnet to pass radio waves through the body. Protons in the body react to the energy and create highly detailed pictures of the body’s structures, including soft tissues, nerves and blood vessels. Unlike X-rays and CT scans, MRIs do not use any radiation.
While some medical facilities have limited diagnostic tools, Texas Back Institute has in-clinic access to all three diagnostic tools and the expertise to use the images safely and accurately for analysis and treatment for conditions such as spinal stenosis.
Physical Therapy and Other Treatment for Spinal Stenosis
Treating spinal stenosis and the resulting nerve compression symptoms involves following the protocol that Texas Back Institute has followed since its formation, more than 45 years ago. Surgery is ALWAYS the last option to be considered. This is true for every neck and back issue, including spinal stenosis.
The first option involves employing conservative care measures. In many cases, these conservative treatments prove to be successful in the alleviation of pain and the restoration of a patient’s quality of life. These measures include prescribing medications for symptoms’ relief, physical therapy and/or injections.
In cases where these conservative options fail, surgery is discussed to solve the problem. In the case of spinal stenosis, the primary problem is the narrowing of the spinal canal. The objective of the surgical procedure is to open up that restricted area of the spine and decompress the nerve roots. In many cases, this procedure is as simple as performing a decompression.
In previous years, this decompression procedure involved midline, larger surgery where tissue was disrupted by the process. This “old-school” type of decompression surgery required more recovery time in order to allow muscle and other tissue to heal. The spine surgeons at Texas Back have been on the forefront of using minimally invasive surgery (link to blog) for this procedure. Now, this surgery is completed by either using tubes or endoscopes and this minimally invasive procedure allows for less tissue disruption and, in most cases, it allows the patient to return home on the same day as the surgery.
Other effective procedures for treating spinal stenosis involve the use of a fusion procedure, where one vertebra is connected, or fused, to another one. This procedure is often used when there are concerns about instability in the spine.
If the patient has a disc pressing on the spine, the surgeon might recommend replacing it with an artificial disc (link to latest ADR blog post). This procedure, which was pioneered by the spine surgeons at Texas Back Institute, has proven to be extremely effective in correcting a disk damaged by spinal stenosis.


Patients Ask:
What type of injections are used in the conservative treatment of spinal stenosis?
Texas Back Institute Responds: In most cases, an epidural injection is prescribed for this type of treatment. An epidural involves injecting a medication — either an anesthetic or a steroid — into the space around the spinal nerves known as the epidural space.

Recovery From Spinal Stenosis Surgery
The advances in diagnostic imaging technology which allow for more accurate location of spinal column restrictions, along with the adoption of minimally invasive surgical procedures have greatly reduced the time necessary for recovery from spinal stenosis procedures. Most patients are allowed to return home on the same day as the surgery and are encouraged to begin walking the day after the procedure.
Typically, most patients can return to regular movements and life after 4 to 6 weeks after surgery. Full results from pain relief might take up to 6 months. During this recovery period, it is recommended that patients recovering from spinal stenosis surgery undergo outpatient physical therapy sessions to learn how to move correctly.
Patients Ask:
When should I consult a spine specialist if I am concerned about the symptoms for spinal stenosis?
Texas Back Institute Responds: Once these symptoms become a hindrance to your quality of life, you should see a spine specialist. Also, if you notice neurological changes such as numbness and weakness or lose bowel or bladder control, it is important to get a thorough examination.
What’s Next?
If spinal stenosis, causing nerve compression and the other symptoms, is ruining your quality of life, there’s good news. It doesn’t have to.
Using state-of-the-art medical technology such as robotics, minimally invasive surgery, artificial disc replacement and other tools, the world class surgeons at Texas Back Institute have successfully diagnosed and treated thousands of patients who were suffering the relentless pain of this debilitating condition.
When you are ready to become pain-free, click here and get your life back.

Learn more
Frequently Asked Questions
A variety of factors can cause spinal stenosis. Disc herniation or bulging can cause narrowing of the canal. Facet joints, which are on the sides of the canal, can also contribute to this condition. As we get older, the wear and tear on these facet joints can lead to what are called bone spurs or cysts which can cause this compression of the nerves. Finally, on the back of the spinal canal, some patients can experience abnormal growth of ligaments which can cause spinal stenosis.
With spinal stenosis, the space around the spinal cord becomes too narrow and this irritates the cord and/or the nerves that come off it. This can lead to tingling and numbness in the extremities of the body.
All spinal stenosis treatments follow the same protocol, starting with a conservative, non-surgical approach and if this is not successful, surgery is discussed. See below.
CT scans, MRIs and X-rays are all diagnostic tools that allow doctors to see the internal structures of the body. They create images using various forms of electromagnetic energy. When used by trained technicians, these tools are safe. However, they are somewhat different in their accessibility, resolution and the type of energy they use for imaging.
An X-ray is the fastest and most accessible form of imaging and this exam only takes a few minutes to complete. However, an x-ray will not show subtle bone injuries, soft tissue injuries or inflammation.
An MRI uses a powerful magnet to pass radio waves through the body. Protons in the body react to the energy and create highly detailed pictures of the body’s structures, including soft tissues, nerves and blood vessels. Unlike X-rays and CT scans, MRIs do not use any radiation.
While some medical facilities have limited diagnostic tools, Texas Back Institute has in-clinic access to all three diagnostic tools and the expertise to use the images safely and accurately for analysis and treatment for conditions such as spinal stenosis.
In most cases, an epidural injection is prescribed for this type of treatment. An epidural involves injecting a medication — either an anesthetic or a steroid — into the space around the spinal nerves known as the epidural space.
Once these symptoms become a hindrance to your quality of life, you should see a spine specialist. Also, if you notice neurological changes such as numbness and weakness or lose bowel or bladder control, it is important to get a thorough examination.
Locations