Osteoporosis: What It Means for Spine Health
how we can help
An Overview of Osteoporosis
Osteoporosis is a bone disease that significantly affects spine health, leading to decreased bone density and increased fragility. This condition progresses silently, often without symptoms until a fracture occurs, making it particularly dangerous for postmenopausal women and older men. Understanding the impact of osteoporosis on the spine is crucial for early detection and prevention of fractures.
As a living tissue, bone is constantly being broken down and replaced throughout life. Unfortunately, as we age, the replacement of this tissue lags behind its destruction. When this happens, bones can become weak and brittle and any type of stress – from a mild fall or even cough or sneeze – can cause these fragile bones to break.
This condition is called osteoporosis, and in the United States an estimated 10 million people aged 50 and older have the condition, according to the federal health resource, Health.gov. Most of these people are women, and about two million are men. Osteoporosis affects all races, but white and Asian women, especially those who are past menopause, are at the highest risk.
Osteoporosis-related breaks most commonly occur in the hip, wrist, or spine. This encourages the spine specialists at Texas Back Institute to pay special attention to those patients who find themselves in the high-risk groups for osteoporosis.
Table of Contents

Symptoms
Diagnosing
Treatments
Patients Ask:
Can osteoporosis be reversed?
Texas Back Institute Responds: While research on this question is on-going, many experts on bone density feel that osteoporosis is not reversible. However, medication, nutrient-dense diet and weight-bearing exercise can help prevent further bone loss and strengthen weaker bones.
The Risk Factors for Osteoporosis
Understanding how people develop osteoporosis is crucial for prevention.
Many people are aware that age, race, and gender are primary risk factors for osteoporosis. However, it may surprise you to learn that there are other, less obvious factors that can lead to this debilitating condition. There are other, less obvious factors that can lead to this debilitating condition. According to the Mayo Clinic, these include:
- Family history
Having a parent or sibling with osteoporosis puts you at greater risk for the condition, especially if your mother or father fractured a hip. A family history of osteoporosis significantly increases the risk of developing the condition.
- Body size
Individuals who have small body frames tend to have a higher risk because they might have less bone mass to draw from as they age.
- Hormone levels: The reduction in estrogen levels in women at menopause is one of the strongest risk factors for developing osteoporosis. Treatments for prostate cancer that reduce testosterone levels in men and treatments for breast cancer that reduce estrogen levels in women are likely to exacerbate bone loss.
- Overactive thyroid: Too much thyroid hormone can cause osteoporosis. This can be the result of an overactive thyroid or from taking too much thyroid medicine to treat an underactive thyroid.
- Inadequate calcium consumption: Many do not get enough calcium in their diets for most of their lives. Inadequate calcium intake can contribute to lower bone density, early bone loss and an increase in the likelihood of fractures.
- Eating disorders that cause underweight status: When food intake is restricted, bones can be weakened.
- Weight-loss surgery: Removing parts of the stomach or intestines limits the surface area that can absorb nutrients such as calcium.
- Corticosteroid medicines: Medicines such as prednisone and cortisone interfere with the bone-rebuilding process.
- Sedentary lifestyle: Those who spend most of their time sitting have a higher risk of osteoporosis than do those who are more active. Any weight-bearing exercise and activities that promote balance and good posture are good for your bones.
- Excessive alcohol consumption: Regular consumption of more than two alcoholic drinks a day increases the risk of osteoporosis.
- Smoking: Research is on-going regarding the exact effect tobacco has on osteoporosis. However, it has been shown that tobacco use contributes to weak bones.
Patients Ask:
Is osteoporosis genetically based?
Texas Back Institute Responds: Yes. A family history which includes osteoporosis is a leading indicator for this condition. What causes osteoporosis is primarily the natural aging process and changes in bone regeneration over time. Bones are living tissues that constantly replace themselves, but after age 35, bone loss increases significantly, and this is even more pronounced in postmenopausal individuals. Those with this family history should begin efforts to offset this trend (for example, making dietary changes to increase calcium intake, reducing, or eliminating tobacco and alcohol and regular exercise) as soon as possible.
The Impact of Osteoporosis on Spine Health
Osteoporosis is the thinning of bone and by itself is not painful. In fact, it is typically associated with aging. Metabolic imbalance, genetics, and medications are also factors.
Osteopenia is a lesser form of this condition and, if not treated, may progress to more serious osteoporosis. In the spine, the thoracic (mid back) and lumbar (low back) segments are the most commonly affected. Osteoporosis leads to significant loss of bone mass, which causes changes in bone tissue, making bones more fragile and susceptible to fractures.
Bone breaks, particularly in the spine or hip, are the most serious complications of osteoporosis. In some cases, broken bones in the spine can occur even if you have not fallen. The bones that make up your spine – the vertebrae – can weaken to the point of collapsing, which can result in back pain, lost height, and a hunched-forward posture.
A hip fracture can lead to serious consequences, such as prolonged bed rest, which increases the risk of other health issues like blood clots and pneumonia.
Vertebral compression fractures occur when the bone weakens and can no longer support the load imposed upon it. Compression fractures in osteoporotic vertebrae can be very painful.
Spinal symptoms related to osteoporosis include neck and back pain and deformity. Individuals with osteoporosis face an increased risk of severe complications, such as fractures and associated mortality.
Patients Ask:
What is a bone density scan and how does it work?
Texas Back Institute Responds: This test is also called a DEXA scan or bone mineral density test. During the process, a large scanning arm will be passed over your body to measure bone density in the center of the skeleton. As the scanning arm is moved slowly over your body, a narrow beam of low-dose X-rays will be passed through the part of your body being examined. The scan usually takes 10 to 20 minutes and you’ll be able to go home after you have had it done.
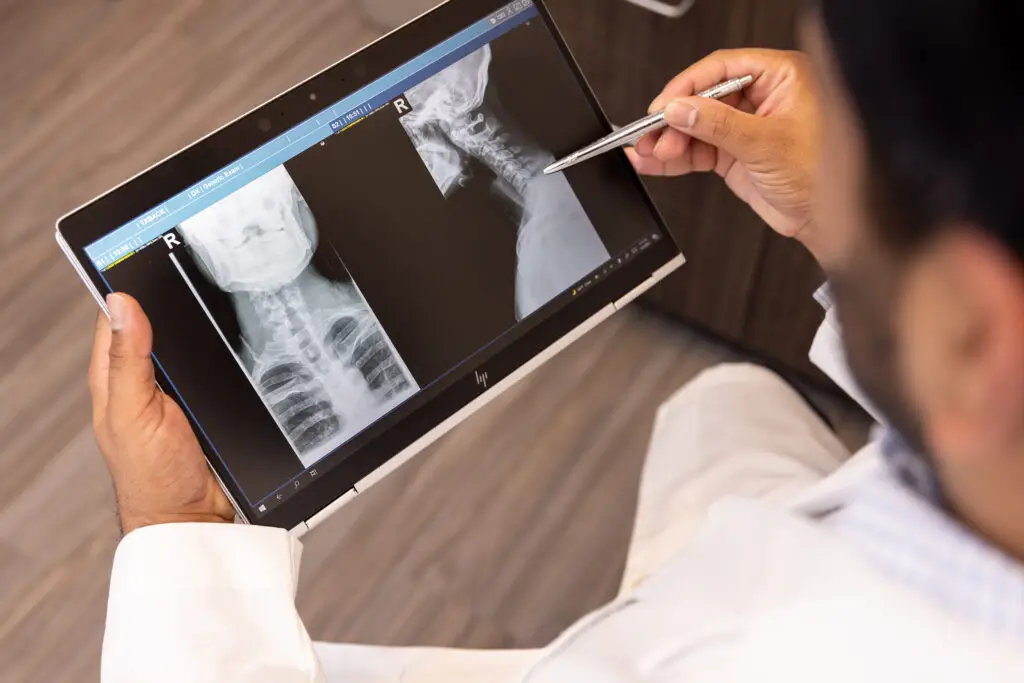
Diagnosing Spinal Osteoporosis
Osteoporosis symptoms are often silent until significant bone loss occurs, making early detection crucial.
After a physical examination, The Texas Back surgeon will take X-rays of the spine to check for fractures. There are several quick-and-easy screening evaluations for osteoporosis that scan the wrist or heel. However, one of the more reliable tests is called the “dual-energy X-ray absorptiometry (DEXA) scan. This diagnostic scan, which is also called a bone mineral density test, is painless and convenient, and it exposes the patient to very little radiation.
Generally, the lower spine and hip are scanned to diagnose osteoporosis. The patient’s bone quality is reported by comparing you to others of the same age and gender as well as to a young adult population.
The results are usually considered in terms of your bone being of normal density, somewhat reduced density (osteopenia), or significantly reduced density (osteoporosis).
Patients Ask:
Can a DEXA scan detect bone cancer?
Texas Back Institute Responds: While a DEXA scan is not typically used to diagnose cancer, it can provide your care team with vital information to help them determine whether additional testing is needed.
Treatment for Osteoporosis
Rebuilding bone density after a lifetime of bone loss is challenging, but not impossible. It requires having excellent medical advice and the commitment to follow a rigorous nutritional and physical regimen to keep bones healthy.
In general, treatment of osteoporosis includes supplementation with calcium and Vitamin D. Weight-bearing exercise, including walking, is extremely important to build stronger bones. However, nutritional experts caution that too much calcium can have unintended and negative consequences.
The Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine recommends that total calcium intake, from supplements and diet combined, should be no more than 2,000 milligrams daily for people older than fifty.
People between the ages of 18 and 50 need 1,000 milligrams of calcium a day. This daily amount increases to 1,200 milligrams when women turn fifty and men turn seventy.
Useful sources of calcium include:
- Low-fat dairy products.
- Dark green leafy vegetables.
- Canned salmon or sardines with bones.
- Soy products, such as tofu.
- Calcium-fortified cereals and orange juice.
If it is difficult to get enough calcium from your diet, some consideration should be given to taking calcium supplements. However, too much calcium has been linked to kidney stones. Although yet unclear, some experts suggest that too much calcium, especially in supplements, can increase the risk of heart disease.
Vitamin D is also on the list for osteoporosis treatment. Nutritional experts note that vitamin D improves the body’s ability to absorb calcium and improves bone health in other ways. In most cases, this vitamin can come from sunlight but too much sun can also have negative impacts such as skin cancer.
Good dietary sources of vitamin D include:
- Cod liver oil,
- Trout and salmon
- Many types of milk and cereal have been fortified with vitamin D.
Most people need at least six hundred international units (IU) of vitamin D a day. That recommendation increases to 800 IU a day after age 70. Vitamin D is essential for maintaining healthy bone tissue and preventing osteoporosis.
In addition to calcium and vitamin D, medications such as bisphosphonates, raloxifene, and parathyroid hormone are available to prevent, reduce, or treat osteoporosis.
A broken bone, especially in older adults, can lead to severe health outcomes, including permanent pain and increased mortality rates. Preventive measures and treatments are crucial to maintain bone health and reduce the risk of fractures.
Exercise, even in moderate amounts, can help build stronger muscles and bone density. The trick is to DO this activity every day. There are excellent exercise programs, such as “Silver Sneakers” offered by the YMCA, which are designed for building muscle and bone density among those who are fifty and older.
The physical therapists at Texas Back Institute suggest anyone older than 50 years should combine strength training exercises with weight-bearing and balance exercises. Many people with osteoporosis indicators forget about balance training, but with age, balance is challenged, and a fall can become a disaster.
Strength training, using free weights or machines, helps strengthen muscles and bones in your arms and upper spine. Before embarking on any type of strength training, it is critical to consult with a qualified trainer or physical therapist.
Weight-bearing exercises such as walking, jogging, running, stair climbing, skipping rope, and skiing and other non-contact activities affect mainly the bones in your legs, hips, and lower spine.
Balance exercises such as tai chi can reduce your risk of falling as you get older.
Patients with conditions like rheumatoid arthritis should manage their treatment carefully to prevent bone loss.
Patients Ask:
Can yoga or planking help those worried about osteoporosis?
Texas Back Institute Responds: Yes. Practicing yoga can increase bone density if done consistently and properly. Yoga also improves balance and flexibility, which can prevent falls and therefore prevent fractures. Exercises like yoga and planking can help prevent hip fractures by improving balance and strength. Planking is a low-impact way to improve core strength and balance.
Start Building Bone Density Now
Healthy bone tissue should appear like a honeycomb with small spaces, which helps prevent osteoporosis by maintaining bone strength and reducing fracture risk.
It is never too late to get stronger and healthier. Using some of these tips can help anyone concerned about osteoporosis to build bone density and keep their spine strong. If you are concerned about osteoporosis, click here to set an appointment for a physical exam and spine check-up.
Learn more
Frequently Asked Questions
While research on this question is on-going, many experts on bone density feel that osteoporosis is not reversible. However, medication, nutrient-dense diet and weight-bearing exercise can help prevent further bone loss and strengthen weaker bones.
Yes. A family history which includes osteoporosis is a leading indicator for this condition. What causes osteoporosis is primarily the natural aging process and changes in bone regeneration over time. Bones are living tissues that constantly replace themselves, but after age 35, bone loss increases significantly, and this is even more pronounced in postmenopausal individuals. Those with this family history should begin efforts to offset this trend (for example, making dietary changes to increase calcium intake, reducing, or eliminating tobacco and alcohol and regular exercise) as soon as possible.
This test is also called a DEXA scan or bone mineral density test. During the process, a large scanning arm will be passed over your body to measure bone density in the center of the skeleton. As the scanning arm is moved slowly over your body, a narrow beam of low-dose X-rays will be passed through the part of your body being examined. The scan usually takes 10 to 20 minutes and you’ll be able to go home after you have had it done.
While a DEXA scan is not typically used to diagnose cancer, it can provide your care team with vital information to help them determine whether additional testing is needed.
Yes. Practicing yoga can increase bone density if done consistently and properly. Yoga also improves balance and flexibility, which can prevent falls and therefore prevent fractures. Exercises like yoga and planking can help prevent hip fractures by improving balance and strength. Planking is a low-impact way to improve core strength and balance.
Locations


