What Is Radiculopathy?
how we can help
Radiculopathy Overview
Radiculopathy is a medical condition that occurs when a nerve root in the spine is compressed, irritated, or damaged. This compression leads to a variety of symptoms, including pain, numbness, tingling, and muscle weakness in the affected area. Radiculopathy can affect any part of the spine, but it is most commonly seen in the cervical (neck) and lumbar (lower back) regions. The condition can be caused by several factors, such as herniated discs, bone spurs, spinal stenosis, and degenerative disc disease. Understanding the underlying cause is crucial for effective treatment and management.
The spine is composed of 33 vertebrae, divided into five regions: cervical, thoracic, lumbar, sacrum, and coccyx. These vertebrae act as a canal for the spinal cord which serves as a kind of communication line from all parts of the body to the brain. This spinal cord “information” is collected by nerve roots that split from the cord and travel between the vertebrae into various areas of the body. In some cases, age-related wear and tear, injuries or disease can cause the nerve roots to become pinched or damaged. The resulting symptoms are called radiculopathy.
These irritated nerve roots which cause radiculopathy cause pain, numbness, tingling, or weakness in the arms or legs. The nerve roots are branches of the spinal cord that carry nerve signals out to the rest of the body at each level along the spine. These include the cervical or neck region, the thoracic mid spine area and the lumbar or low back region. While neck and back pain, especially lower back pain, are common issues that may coexist with radiculopathy, they are often not the primary cause of radiculopathy. Arm and leg, and more specific radicular symptoms are the primary manifestation of this condition.
Radiculopathy is often caused by direct pressure from a herniated disc, bone spur, or degenerative changes in the spine that cause the collapse of the nerve root tunnels which are also called foramena.
With this condition, sensory symptoms such as numbness, pins and needles, tingling, crawling, prickling, burning, tightness or itching, and pain are more common than motor symptoms which affect your movement and balance such as muscle weakness, tremor, stiffness, and slowness of movement. As such muscle weakness is usually a sign that the nerve compression is more severe. The quality and type of pain resulting from radiculopathy can vary, from dull, aching, and difficult to localize, to sharp and burning.
Table of Contents
Symptoms
- Cervical: Neck, shoulder, arm, or hand pain.
- Thoracic: Pain wrapping to chest/abdomen.
- Lumbar: Lower back to leg pain (sciatica).
Diagnosing
- X-rays: Identify structural issues.
- MRI or CT scans: Locate nerve root compression and assess soft tissues.
Treatments
Patients Ask:
What is the difference between radiculopathy and neuropathy?
Texas Back Institute Responds: These two conditions are similar in that they are both related to nerve damage and have similar symptoms. However, while radiculopathy is caused by the pinching of root nerves of the spinal column, neuropathy is damage or malfunction of peripheral nerves.
Three Types of Radiculopathy
There are three types of radiculopathy and they are related to the region of the spine in which they occur. Radiculopathy symptoms can vary depending on the type and location of the radiculopathy.
Lumbar Radiculopathy
According to the spine specialists at Texas Back Institute, radiculopathy occurring in the low back is known as lumbar radiculopathy. Acute lumbar radiculopathy requires effective treatment methods that address the underlying causes and restore nerve function. This condition is also referred to as sciatica because nerve roots that make up the sciatic nerve are often involved. The lower back is the area most frequently affected by radiculopathy.
Cervical Radiculopathy
Cervical radiculopathy describes a compressed nerve root in the neck (cervical spine). Because the nerve roots in this area of the spine primarily control sensations in your arms and hands, this is where the symptoms are most likely to occur.
Thoracic Radiculopathy
Thoracic radiculopathy refers to a compressed nerve root in the thoracic area of the spine, which is your upper back. This is the least common location for radiculopathy. The symptoms can cause pain and numbness that wraps around to the front of the body.

Patients Ask:
How does radiculitis differ from radiculopathy?
Texas Back Institute Responds: They are related conditions, however most people with radiculopathy can find relief through treatment. Radiculitis is also caused by damage to the nerves. However, radiculitis is typically much more severe and causes inflammation in addition to the other symptoms of radiculopathy.
What Causes Radiculopathy?
The spine experts at Texas Back Institute note that radiculopathy is usually caused by changes in the tissues surrounding the nerve roots. These tissues include bones of the spinal vertebrae, tendons, and intervertebral discs.
When these tissues shift or change in size, they may narrow the spaces where the nerve roots travel inside the spine or exit the spine. These openings are called foramina, and the narrowing of foramina is known as foraminal stenosis. This condition is similar to spinal stenosis that affects the spinal cord.
In most cases, foraminal stenosis is caused by gradual degeneration of the spine that is the age-related wear and tear. However, it can also be a result of a spinal injury, and these can include the following:
Herniated Discs
One common cause of foraminal stenosis and radiculopathy is a bulging or herniated disc. Spinal discs act as cushions between vertebrae, and they can slip out of place or become damaged and press on nerves. This problem is most likely to occur in your lower back (lumbar area), but it can also affect your neck or cervical region of the spine.
Bone Spurs
Another possible cause of radiculopathy that may lead to narrowing of foramina is bone spurs. These are areas where extra bone growth has occurred. Bone spurs can form in the spine due to inflammation from osteoarthritis, trauma, or other degenerative conditions.
Other Causes
When ossification or thickening of the spinal ligament occurs, this can cause a narrowing of the space around the nerve roots and compression of the nerves. Spinal infections and various cancerous and noncancerous growths in the spine that may press against the nerve roots can cause radiculopathy, but these are uncommon.
Patients Ask:
What are the symptoms of radiculopathy?
Texas Back Institute Responds: When a nerve root is compressed, it becomes inflamed. This results in several radiculopathy symptoms including:
- Sharp pain in the back, arms, legs, or shoulders that may worsen with certain activities, even something as simple as coughing or sneezing
- Weakness or loss of reflexes in the arms or legs
- Numbness of the skin, “pins and needles,” or other abnormal sensations in the arms or legs
Specific symptoms will depend on where in the spine the nerve root is pinched. It is also possible that you don’t experience any symptoms, or you go through periodic flare-ups of symptoms.

How Radiculopathy Is Diagnosed
The correct diagnosis for radiculopathy begins with a complete physical examination of the neck, back, arms, and lower extremities. The spine specialist will check for any problems with flexibility, muscle strength, sensation, and reflexes.
X-rays may be indicated to show the bony anatomy of the spine. An MRI scan or a CT scan may also be ordered. An MRI scan is useful in showing compression of nerve roots by giving a detailed picture of soft tissue structures.
A CT scan is often used to evaluate the bony anatomy in the spine, which can show how much space is available for the nerve roots and spinal cord within the spinal canal. Early on, in mild situations, imaging studies may not be required.
Nerve conduction study, along with electromyography, can also be used to help pinpoint whether the problem is neurological or muscular. This test measures how fast an electrical impulse moves through your nerve, and it can identify nerve damage.
During the test, a nerve is stimulated with electrode patches put on the skin. Two electrodes are placed on the skin over your nerve or over a muscle. One electrode stimulates your nerves with a very mild electrical impulse. The other electrode records it.
The resulting electrical activity is recorded by another electrode. This is repeated for each nerve being tested. The speed is then calculated by measuring the distance between electrodes and the time it takes for electrical impulses to travel between electrodes.
An electromyography (EMG) test measures the electrical activity in your muscles. Both tests help determine the presence, location, and extent of diseases that damage the nerves and muscles.
Patients Ask:
What is lumbosacral radiculopathy?
Texas Back Institute Responds: The National Institute of Health notes that Lumbosacral radiculopathy is characterized by pain resulting from compression or irritation of nerve roots in the lumbosacral region of the spine, along with numbness, weakness, and reflex changes. This condition can manifest without overt lumbar pain, making its recognition crucial for timely intervention. The condition often arises due to degenerative changes such as disc herniation, ligamentum flavum changes, facet hypertrophy, or spondylolisthesis, leading to nerve root compression.
How Is Radiculopathy Related to Myelopathy
Sometimes, radiculopathy can be accompanied by myelopathy which is the compression of the spinal cord itself.
What causes myelopathy? With age, inflammation, arthritic illness, bone spurs and the flattening of the spinal discs between the vertebrae can put pressure on the spinal cord and the nerve roots. In most cases, myelopathy develops slowly as result of the gradual degeneration of the spine, which is also known as spondylosis, but it can also take an acute form or stem from a spine deformity present at birth.
Common causes of myelopathy are:
- Degenerative spinal conditions, such as spinal stenosis which is a narrowing of the bony passageways of the spine through which the spinal cord and nerve roots travel.
- Central disk herniations can also result in compression on the spinal nerve root, leading to the development of myelopathy.
- Autoimmune disorders, such as rheumatoid arthritis in the spine, can also lead to degenerative changes in the vertebrae that result in spinal cord compression and myelopathy.
- Hernias, cysts, hematomas, and spinal tumors, including bone cancer, may also press on the spinal cord and lead to myelopathy.
Herniated or bulging discs can sometimes press on the spinal nerve root. When the spinal cord is involved, the symptoms can be more severe, including poor coordination, trouble walking and paralysis.
(Insert TBI YouTube video to be determined featuring physician discussing radiculopathy)
Patients Ask:
How does radiculopathy differ from a “pinched nerve?”
Texas Back Institute Responds: Essentially, the two terms are interchangeable. Pinched nerves can occur nearly anywhere in the body, from the neck, low back and spine to the wrists. Cervical radiculopathy (also known as “pinched nerve”) is a condition that results in neurological dysfunction caused by compression and inflammation of any of the nerve roots of the cervical spine (neck). Neurological dysfunction can include radiating pain, muscle weakness and/or numbness.
How Radiculopathy Is Treated?
Conservative, non-surgical treatment is always the first option patients should be given in dealing with radiculopathy. Physical therapy, chiropractic manipulation, patient education, and non-steroidal anti-inflammatory medication are the most common non-invasive treatment options for most patients with no evidence of significant muscle weakness caused by radiculopathy. Weight-loss programs and lifestyle modifications such as smoking secession can also be helpful in dealing with this condition.
Epidural steroid injections may also be considered for severe cases. An epidural is a procedure that involves injecting a medication — either an anesthetic or a steroid — into the space around spinal nerves known as the epidural space. The goal of an epidural procedure is to provide pain relief or a complete lack of feeling for one region of your body, such as your legs or belly.
Muscle weakness is a concerning sign of nerve root compression or radiculopathy. Nerve testing (electromyography or EMG) may be indicated to objectively test the condition of the nerve-muscle connection, particularly if strength testing is limited by pain.
If a patient suffers from an actual nerve injury, surgery may be required. Surgery for radiculopathy is typically used to reduce the pressure on the nerve root by widening the space where the nerve roots exit the spine. This may involve removing all or parts of a disc and/or vertebrae. Cervical posterior foraminotomy is one of the minimally invasive spine surgery options available.
At Texas Back Institute, surgery is always the final option to consider and is only recommended when non-surgical treatment options have failed to improve the symptoms of radiculopathy. It is important to discuss treatment options with your doctor in deciding which treatment, if any, may be best for you.
What That Pain Is Telling You?
The feeling of acute pain is usually sharp because it tends to act as a warning signal about a threat to the body from an injury, disease, overuse, or other environmental stress. If you are getting that warning signal, it could be serious or minor. Either way, it is always advisable to listen and get an expert opinion. If that pain is related to your neck or back, click here to talk to the spine experts at Texas Back Institute.
Learn more
Frequently Asked Questions
These two conditions are similar in that they are both related to nerve damage and have similar symptoms. However, while radiculopathy is caused by the pinching of root nerves of the spinal column, neuropathy is damage or malfunction of peripheral nerves.
They are related conditions, however most people with radiculopathy can find relief through treatment. Radiculitis is also caused by damage to the nerves. However, radiculitis is typically much more severe and causes inflammation in addition to the other symptoms of radiculopathy.
When a nerve root is compressed, it becomes inflamed. This results in several radiculopathy symptoms including:
- Sharp pain in the back, arms, legs, or shoulders that may worsen with certain activities, even something as simple as coughing or sneezing
- Weakness or loss of reflexes in the arms or legs
- Numbness of the skin, “pins and needles,” or other abnormal sensations in the arms or legs
Specific symptoms will depend on where in the spine the nerve root is pinched. It is also possible that you don’t experience any symptoms, or you go through periodic flare-ups of symptoms.
The National Institute of Health notes that Lumbosacral radiculopathy is characterized by pain resulting from compression or irritation of nerve roots in the lumbosacral region of the spine, along with numbness, weakness, and reflex changes. This condition can manifest without overt lumbar pain, making its recognition crucial for timely intervention. The condition often arises due to degenerative changes such as disc herniation, ligamentum flavum changes, facet hypertrophy, or spondylolisthesis, leading to nerve root compression.
Essentially, the two terms are interchangeable. Pinched nerves can occur nearly anywhere in the body, from the neck, low back and spine to the wrists. Cervical radiculopathy (also known as “pinched nerve”) is a condition that results in neurological dysfunction caused by compression and inflammation of any of the nerve roots of the cervical spine (neck). Neurological dysfunction can include radiating pain, muscle weakness and/or numbness.
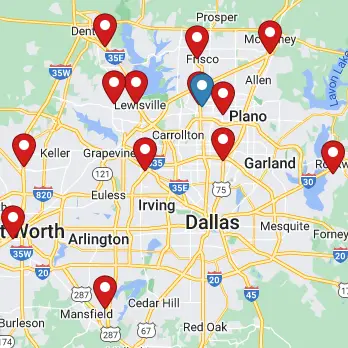
Locations