Balancing Stability and Motion: Dynamic Stabilization Surgery
how we can help
Dynamic Stabilization Surgery Overview
Spinal instability is a broad term used to describe the occurrence of abnormal movement or alignment between the spinal vertebrae. It can be caused by many factors, including degenerative changes in the spine, infections, tumors, trauma, or genetic abnormalities. The movement of these discs can cause irritation or discomfort in the affected area. There are several procedures that can restore stability to the affected spinal segment, including spinal fusion and dynamic stabilization surgery, or DSS.
Dynamic stabilization surgery is an alternative to spinal fusion surgery. The purpose of dynamic stabilization surgery is stabilization of the spine, while preserving a greater degree of flexibility. Instead of fusing the discs together, this procedure involves implanting a device at the affected area that gives the spine a greater degree of flexible motion. Some dynamic stabilization devices can be implanted using minimally invasive surgical techniques.
Spinal fusion surgery is considered the “gold standard” for treatment of spinal instability. Spinal fusion surgery stabilizes the spine by fusing two adjacent vertebrae together, eliminating abnormal movement at the fused level. Although there’s some loss of flexibility where the vertebrae are fused, back pain, numbness, and weakness due to spinal instability are greatly reduced.
According to an article in the Journal of Neurosurgery, “dynamic stabilization surgery offers an alternative to fusion, aiming to balance stability and motion while reducing surgical complexity. Both approaches have their merits, and the choice depends on individual patient factors.” Basically, the purpose of both procedures is to restore stability to the spine.
Table of Contents

Treats
Diagnosing
Recovery
Patients Ask:
I have symptoms of spinal instability. Which procedure is right for me?
Texas Back Institute Responds: The choice between spinal fusion surgery and dynamic stabilization surgery depends on the specific patient’s condition. The spine specialists at Texas Back Institute make individual assessments and recommendations based on the potential benefits and drawbacks of each procedure.
What Causes Spinal Instability?
The bones, spinal disks, ligaments, and muscles in the spine all work in combination to support and protect the spinal cord. When spinal instability occurs, supporting structures may be weakened or damaged. If this happens, it can lead to abnormal movement, causing excessive stress on the spine and compression of the spinal cord and nerve roots.
Spondylolisthesis is a condition in which a vertebra slips out of alignment, moving forward on the vertebra below. Spondylolisthesis is usually caused by a degenerative disease, such as osteoarthritis, but can also result from a congenital disorder of the spine. High impact sport activities can also result in abnormal movement in the spine. For example, gymnasts, weightlifters, and football players are all at an increased risk.
Some causes of spinal instability include:
- Degenerative Disk Disease: Spinal disks can break down from “wear and tear.” Over time, this can contribute to spinal instability.
- Herniated Disks: When the inner portion of a spinal disk bulges out, it can affect spinal stability.
- Spinal Stenosis: This is the narrowing of the space around the spinal cord and this condition can lead to instability.
- Osteoarthritis: This refers to the degeneration of the spinal column due to aging, which can weaken spinal stability.
- Congenital abnormalities: Some people are born with spinal defects that can impact spinal stability.
- Scoliosis: Abnormal spinal alignment can contribute to spinal instability.
- Trauma: External injuries can cause spinal instability.

Patients Ask:
What are some symptoms of spinal instability?
Texas Back Institute Responds: A spine segment is unstable if it moves in an abnormal way under normal physiologic loads. There is a spectrum of symptoms that can result from spinal instability. Spine specialists would expect pain in the injured area and nerve compression that causes pain, numbness or weakness in the arms or legs. If the spinal cord is compressed it could cause profound numbness, paralysis or the inability to walk, profound weakness, and loss of control in bladder or bowel function.

Anatomy of the Lumbar Spine
Although the lumbar spine is strong and durable, it is subject to a high degree of stress and physiologic loads, which can result in degenerative “wear and tear” and eventually lead to spinal instability.
The lumbar spine consists of five vertebrae, known as L1 to L5. Compared to the rest of the spine, the lumbar vertebrae are the largest vertebrae, responsible for supporting most of the body’s weight. The lumbar spine is also the body’s center of balance.
Intervertebral disks act as “shock absorbers” that cushion each vertebra. Five disks are positioned between the vertebrae in the lumbar spine. In addition, intervertebral disks function to help support body weight by bearing the physiologic load coming down the spine and allowing movement between each vertebra. Disks in the lumbar region are the most likely to degenerate or herniate, which then causes pain in the low back or nerve pain that radiates down to the legs and feet.
Ligaments in the lumbar spine connect bone to bone to help to keep the spine stable, flexible and able to absorb the force of trauma. Lumbar spine ligaments include:
- Anterior longitudinal ligament
- Posterior longitudinal ligament
- Supraspinous ligament/interspinous ligament
- Ligamentum flavum
- Intertransverse ligament
- Iliolumbar ligament.
The spinal cord is a bundle of nerve tissue that extends from the lower part of the brain to the L1 vertebra, carrying messages between the brain and muscles. The remaining nerve roots are below the spinal cord. Called the cauda equina, these nerves travel down the rest of the spinal canal.
The lumbar spine has five pairs of spinal nerves that branch off from the right and left sides of L1 to L5 vertebrae. These spinal nerves travel from the lower back and merge with other nerves to form a network of nerves controlling pain signals and movement in the lower extremities.
- The L1 spinal nerve provides sensation to the groin and genital area and helps move the hip muscles.
- L2, L3 and L4 spinal nerves provide sensation to the front part of the thigh and inner side of the lower leg, controlling hip and knee muscle movements.
- The L5 spinal nerve provides sensation to the outer side of the lower leg, the upper part of the foot and the space between the first and second toe. This nerve also controls hip, knee, foot and toe movements.
- The sciatic nerve consists of the L4 and L5 nerves, plus other sacral nerves. The sciatic nerve starts in the rear pelvis and runs down the back of the leg, ending in the foot.
Muscles in the lumbar spine help stabilize, rotate, flex, and extend the spinal column. They include:
- Multifidus: This long muscle travels nearly the entire length of the back. It stabilizes and rotates the lumbar spine.
- Longissimus: Another long muscle, this one begins in the middle of the lumbar spine and continues up to the transverse process.
- Quadratus Lumborum: This muscle is part of the posterior group of muscles in the lumbar spine.
- Psoas Major and Minor: These are part of the flexor group of muscles.
- Internal and External Oblique: These muscles are also part of the flexor group.
- Rectus Abdominis: This is another muscle in the flexor group.
- Interspinales Lumborum and Erector Spinae (Iliocostalis, Longissimus): These are part of the extensor group.
- Latissimus Dorsi: This muscle attaches to the lumbar spine.
Patients Ask:
How is spinal instability in the low back diagnosed?
Texas Back Institute Responds: A complete history and physical exam is always the first part of a diagnostic workup for any painful condition. Usually, spinal x-rays will be obtained to check for instability. You will likely be asked to flex forward and extend backward for different x-rays so that your surgeon can evaluate whether the bones move abnormally when you change body positions. More advanced imaging studies such as a CT scan or an MRI scan may also be ordered to get additional information about the amount of nerve compression that may be resulting from the instability and to see whether there are any fractures in the bony structures.
Dynamic Lumbar Stabilization Surgery
Dynamic lumbar stabilization surgery is performed as an alternative to spinal fusion to improve stability, reduce pain, decompress nerves, and correct deformities in the lumbar region. By stabilizing the spinal column, abnormal motion of the spinal segments is limited. A flexible and sturdy titanium device called a Coflex® is inserted between the lamina to provide support, relieve pressure, and preserve motion. The device is inserted in between and attaches above and below the spinous processes, a small projection of bone that points outward from each vertebra along the spine.
Decompression with an Interlaminar Stabilization® device relieves the pain associated with spinal stenosis. Once the nerve has been decompressed the surgeon will insert the Coflex device to stabilize the spine and maintain the decompression without limiting motion. The Coflex Interlaminar Stabilization procedure is used to treat moderate to severe spinal stenosis. The Coflex device is a single-piece titanium implant that goes in the back of the spine to support and preserve lumbar motion. This technique also reduces the load on the spine’s joints and discs, which may reduce pain and improve the recovery time after the surgical procedure.
Dynamic stabilization surgery has the advantage of potentially reducing some of the problems associated with metal implants, such as disk degeneration adjacent to the fusion site.
Patients Ask:
If my surgeon thinks I am a good candidate, what should I expect?
Texas Back Institute Responds: Cervical arthroplasty is a relatively safe procedure. Surgeons make an incision on the front of the neck, just off of midline – which is relatively pain free since only a small incision is necessary. The trachea and esophagus are moved to the side and blood vessels are moved allowing the diseased disc to be removed using magnification and ensuring that the spinal cord and all the nerves are completely decompressed.
The artificial disc is then implanted using an intraoperative x-ray so that it’s positioned appropriately. The incision is closed with dissolvable sutures. Patients may be given a soft collar to wear to help protect the wound. Some patients stay at the hospital overnight, especially if they are having multiple levels done, but many times patients can go home the same day.
Types of Dynamic Stabilization Surgery
Dynamic spinal stabilization doesn’t apply to any one surgery. It’s a general term for procedures that restore the stability of the spine while maintaining some degree of flexibility.
Procedures that fall under this category include:
- Dynamic rods soft stabilization
This involves the use of flexible rods to stabilize the spine while allowing some movement.
- Dynamic screws
These are special screws that allow a certain degree of movement.
- Dynamic rods and dynamic screws in combination
This approach uses both dynamic rods and screws to stabilize the spine.
- Facet function replacing ball-and-socket joint
This procedure replaces the facet joints in the spine with artificial ball-and-socket joints to allow movement.
- Total facet joint replacement
This involves the complete replacement of the facet joints in the spine.
- Facet augmentation
This procedure strengthens the facet joints in the spine.
- Interspinous device
This involves the placement of a device between the spinous processes in the spine to provide stability.

Minimally Invasive Dynamic Lumbar Stabilization Surgery
Dynamic lumbar stabilization surgery can be performed as a minimally invasive procedure. Surgeons perform the procedure through a small incision in the back or side. A small metal tube or endoscope passes through the incision to allow the surgeon to work through a smaller operating field, resulting in much less damage to muscles, soft tissues and skin. Recovery time is usually shorter with this procedure.
Patients with symptoms such as numbness, weakness, or pain in the lower legs, difficulty walking long distances, and lower back pain that improves when bending over or sitting down are good candidates for this type of procedure. It’s used to treat spinal stenosis with instability or potential instability caused by conditions like bone spurs, ligament thickening, or collapsing disc heights in the lower spine without the invasiveness and loss of flexibility associated with spinal fusion.
Patients Ask:
What is the recovery time for this procedure?
Texas Back Institute Responds: The recovery time for minimally invasive dynamic lumbar stabilization surgery can vary depending on several factors including the patient’s overall health, the specific procedure performed, and how well the patient follows post-operative instructions. During the first 3 months of recovery, patients should avoid long drives, sitting and standing for long periods, and lifting. Most patients may resume sedentary desk work within 2-4 weeks, and moderate duty within 6 weeks.
Combining Spinal Procedures
Dynamic stabilization devices have been approved for use as an accessory to spinal fusion, adding stability to the spine and helping to maintain proper spinal alignment while the fusion becomes solid.
The advantage to combining both procedures is that the dynamic stabilization implant is much less rigid. Allowing a small amount of motion can help to prevent degeneration of the adjacent discs and facets and can stabilize posterior destabilizing surgeries such as wide laminectomy and facetectomy. In some cases, a dynamic stabilization procedure with spinal fusion will allow the retention of the bony plate of each vertebral body, typically removed during a spinal decompression procedure.
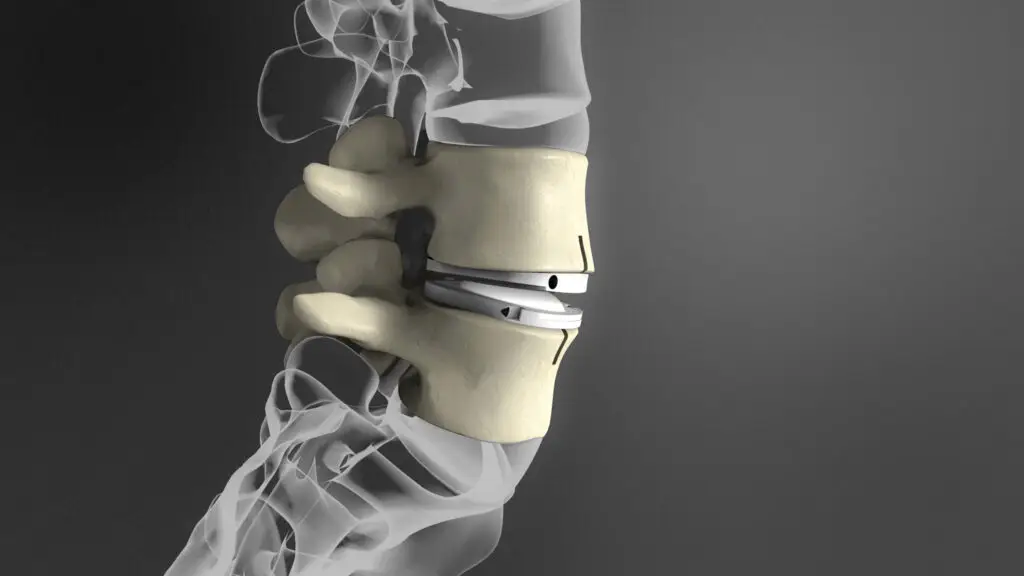
Dynamic and Stabilizing: Artificial Disc Replacement
Pioneers in the field of spinal surgery, Texas Back Institute performed the first lumbar disc replacement in the United States in March 2000. Artificial disc replacement (ADR) offers patients pain relief while preserving the spine’s mobility, making it an optimal solution for chronic pain, degenerative disc disease, and herniated discs.
Unlike traditional fusions, where material or bone grafts are placed between vertebral bodies to eliminate motion, artificial disc replacement removes the cause of pain by replacing the disc and preserving motion. Advances have also led to discs that mimic our normal discs, providing compressibility and shock absorption. Long-term studies show that disc replacement reduces the chance of needing future surgery compared to fusion.
In the past, spinal fusion was the most common procedure used to eliminate pain from degenerative disc disease. In fusion surgeries, the disc is removed and replaced by bone. The vertebrae are fused together, eliminating movement, and significantly reducing pain in the area. ADR (https://texasback.com/how-has-artificial-disc-replacement-evolved-after-20-years/) allows for the normal, or close to normal, movement of the spine. Recovery is generally much faster than with spinal fusion as well.
Patients Ask:
Am I a good candidate for ADR surgery?
Texas Back Institute Responds: People who do not see improvement from conservative care, including medication, injections, chiropractic therapy, and physical therapy, will most likely be recommended for artificial disc replacement surgery or spinal fusion. Texas Back Institute spine specialists will use an MRI to determine the amount of degeneration, and discography will be used to pinpoint exactly where the problem lies. Discography is the process of injecting dye into the discs and taking x-rays and a CT scan to examine which discs are related to your pain. Certain medical conditions may prevent you from being a good candidate for ADR surgery. People with spondylolisthesis, osteoporosis, fractures of the vertebrae, a spinal tumor, spinal infection, or allergies to artificial materials, and those who are pregnant or morbidly obese will not be recommended for ADR surgery.
Nonsurgical Interventions
As always, the spine specialists at the Texas Back Institute only recommend surgery as a last resort. Therapeutic interventions for spinal instability begin with a program of conservative care treatments that may include:
- Pain Management: nonsteroidal anti-inflammatory medication and steroid injections (epidural steroids) to reduce inflammation and reduce pain.
- Physical Therapy: PT will focus on a combination of exercises, posture correction, and pain management techniques. Specific exercises can help strengthen the muscles that support the spine and improve flexibility.
- Hot and Cold Therapy: Ice can be used to temporarily help with any swelling or temporary pain relief. Heat can relax the muscles or increase blood flow and may help temporarily with pain.
- Lifestyle Modifications: These may include weight reduction, limited activity, and avoiding activities that exacerbate pain. Patients are urged to avoid smoking and excessive alcohol consumption.
- Back Braces: Braces can provide support, stability, and pain relief.

Next Steps?
Ignoring back pain can lead to potentially serious complications such as chronic pain, nerve damage, loss of function and mobility, or bowel and bladder dysfunction. Without treatment, back pain could spread to other areas, like the hips or legs. Without treatment, there is a possibility that damage could become irreversible.
If you are experiencing symptoms, the best course of action is to seek prompt medical attention. Early diagnosis can prevent these potential consequences from occurring and you can get back to living your life pain-free!
If back pain is affecting your life, it doesn’t have to. Click here to schedule an appointment with the specialists at Texas Back Institute.
Learn more
Frequently Asked Questions
The choice between spinal fusion surgery and dynamic stabilization surgery depends on the specific patient’s condition. The spine specialists at Texas Back Institute make individual assessments and recommendations based on the potential benefits and drawbacks of each procedure.
A spine segment is unstable if it moves in an abnormal way under normal physiologic loads. There is a spectrum of symptoms that can result from spinal instability. Spine specialists would expect pain in the injured area and nerve compression that causes pain, numbness or weakness in the arms or legs. If the spinal cord is compressed it could cause profound numbness, paralysis or the inability to walk, profound weakness, and loss of control in bladder or bowel function.
A complete history and physical exam is always the first part of a diagnostic workup for any painful condition. Usually, spinal x-rays will be obtained to check for instability. You will likely be asked to flex forward and extend backward for different x-rays so that your surgeon can evaluate whether the bones move abnormally when you change body positions. More advanced imaging studies such as a CT scan or an MRI scan may also be ordered to get additional information about the amount of nerve compression that may be resulting from the instability and to see whether there are any fractures in the bony structures.
The recovery time for minimally invasive dynamic lumbar stabilization surgery can vary depending on several factors including the patient’s overall health, the specific procedure performed, and how well the patient follows post-operative instructions. During the first 3 months of recovery, patients should avoid long drives, sitting and standing for long periods, and lifting. Most patients may resume sedentary desk work within 2-4 weeks, and moderate duty within 6 weeks.
People who do not see improvement from conservative care, including medication, injections, chiropractic therapy, and physical therapy, will most likely be recommended for artificial disc replacement surgery or spinal fusion. Texas Back Institute spine specialists will use an MRI to determine the amount of degeneration, and discography will be used to pinpoint exactly where the problem lies. Discography is the process of injecting dye into the discs and taking x-rays and a CT scan to examine which discs are related to your pain. Certain medical conditions may prevent you from being a good candidate for ADR surgery. People with spondylolisthesis, osteoporosis, fractures of the vertebrae, a spinal tumor, spinal infection, or allergies to artificial materials, and those who are pregnant or morbidly obese will not be recommended for ADR surgery.
Locations


