Spinal Fusion Surgery: The Benefits and Limitations
how we can help
An Overview of Spinal Fusion Surgery
Spinal Fusion is a surgical procedure performed to “fuse” two or more vertebrae together. This procedure is done with the use of bone graft material and surgical hardware such as plates, rods, or screws to allow healing of the affected area as one solid unit.
Fusion surgery is performed to help reduce back pain or neck pain resulting from several diagnoses, discussed below. This surgery is considered only after conservative measures have not provided significant relief. There are two spinal fusion surgeries: cervical spinal fusion or neck fusion and lumbar fusion surgery or low back fusion surgery (also known as lumbar spinal fusion).
Understanding the process and benefits of spinal fusion surgery involves a better understanding of the “architecture” of the spine. The spine is made up of interconnected bones which are called vertebrae. These bones start at the base of the skull and conclude at the tailbone at the lower back. Each bony vertebrae sits on top of one another, forming the vertebral column.
Separating these vertebral bodies are disc “cushions” that act as “shock absorbers” for these bones as the body is moving. These discs also permit the bending and twisting motion of the spine, along with the help of facet joints. Protected within the spinal column is the spinal cord that connects the brain to the rest of the entire body. Spinal nerves arise from this nerve bundle in pairs, one on every side of the vertebra.
There are several ways to fuse a spinal segment and these fusion procedures depend on the individual’s pain complaints, history of previous surgery, medical health, and spinal structure. The number of levels (how many vertebrae) involved in the fusion depends on the disc levels identified as problematic through diagnostic studies prior to surgery. The particular fusion graft or device to use during surgery will be determined by the surgeon. This decision is based upon individual anatomy, levels of involvement, patient’s medical health, and overall patient safety.
Spinal fusion is designed to reduce movement and immobilize the affected vertebrae making the spine more stable. This is a “double-edged sword,” with many positive and some negative aspects for patients. Spinal fusion surgery enhances the stability of damaged or weakened vertebrae, but it also reduces flexibility of movement. This technique helps prevent further compression or damage to the spinal cord and nerves by decreasing the added stress that may accelerate with the progression of wear and tear.
Spinal fusions are prevalent in the United States, with thousands of procedures performed annually, highlighting their significance in treating various spinal conditions. For more than 45 years, the spine surgeons at Texas Back Institute have pioneered and perfected spinal fusion surgery and thereby dramatically improved the quality of life for patients who have experienced the symptoms of spinal instability.
Table of Contents
Treats
Diagnosing
Recovery
Patients Ask:
What is Anterior Cervical Fusion (ACF)?
Texas Back Institute Responds: ACF is a procedure that stabilizes the back by grafting any number of the 2 to 7 vertebrae together. This prevents motion and eases pain. As patients heal, the graft and vertebrae grow together. It is called “anterior cervical fusion” because the procedure is done from the front of the neck. The acronym, PCF, refers to a similar fusion procedure that is done from the back, or posterior, part of the neck.
The History of Spinal Fusion Surgery
Spinal fusion surgery has a rich medical history, going back to the late 1800s. It developed because of the severity of spine diseases that physicians were forced to deal with during this period.
According to the National Institute of Health, the “spinal disease physicians faced in the late nineteenth century can hardly be overstated: traumatic injuries, congenital defects, and tuberculosis or Pott’s disease often resulted in severe neurologic impairment and global disability. With the advancements in antiseptic surgery and innovations in anesthesia by William T.G. Morton, bold surgeons dared to help patients suffering from spinal deformity.
“In the 1890s, W.T. Wilkins described treating a newborn with spina bifida. Upon dissection, he found that ‘the last dorsal and the first lumbar vertebra were . . . separated by a half-inch and a hernia protruded through the fissure. The hernia was reduced, and the two vertebrae were held together by a figure-of-8 carbolized silk ligature.’
“An American surgeon, Berthold Earnest Hadra, attempted to treat a patient with progressive neurologic decline from a fracture dislocation of the cervical spine. In 1891, he described using a wire to bring together the sixth and seventh cervical vertebrae for stability.
“In the early twentieth century, two giants in spine surgery, Russell Hibbs and Fred Albee, pushed the boundaries of science to treat patients suffering from Pott’s disease. Hibbs’s original technique involved treating a 9-year-old boy with a kyphotic deformity by removing the spinous processes and laying them down over the interspinous space to promote fusion and repairing the periosteum over the fusion mass. In this period, Albee, citing his experimental works on dogs, proposed using bone grafting to enhance spinal fusion in patients suffering from Pott’s disease.
“In modern times, pedicle screws, interbody devices, and osteoinductive and osteoconductive bone grafts all work to assist in forming a solid fusion mass.
Techniques in spinal fusion have advanced exponentially over the past 25 to 50 years, as has understanding of the biology and biomechanics surrounding spinal fusion. As we reflect on this history, we must also look forward to how spinal fusion will change over the next 50 years.”
If history is any indication, the future of spinal fusion is bright. With the remarkable diagnostic tools, computer enhanced imaging, surgical robotics and the exemplary surgical training that spine surgeons like those at Texas Back Institute employ, will continue to change the lives of patients suffering from spinal disease and injury.

Patients Ask:
What are ALIF and TLIF spinal fusion procedures?
Texas Back Institute Responds: ALIF or Anterior Lumbar Interbody Fusion, is an approach to spinal fusion surgery where the surgeon accesses and repairs the lower (lumbar) spine from the front (anterior) of the patient’s body. This is usually accomplished through a lower abdominal incision. A TLIF procedure is a Transforaminal Interbody Lumbar Fusion. It treats spinal instability or weakness by permanently uniting bones of the lumbar (lower) spine. TLIF spine surgery is generally less invasive than a posterior spinal fusion (PLIF) with regards to lumbar spinal fusion surgery, but it can sometimes be less effective.

Injuries or Disease That May Suggest Spinal Fusion Surgery
There are at least three primary reasons the spine surgeons at Texas Back Institute might recommend spinal fusion surgery. These are: (1) making the spine more stable, (2) correcting a problem in the spine caused by disease or injury, and (3) reducing pain that is caused by disease or trauma from injury.
Spinal fusion can be used to:
- Correct a fractured spine or broken vertebra
This can result from automotive or other accidents.
- Reshape the spine
Spinal fusion can help correct problems with the way the spine is formed. An example of this is scoliosis, when the spine curves sideways causing deformity.
- Correct spinal weakness or instability
Too much motion between two spinal bones can make the spine unstable. This is a common side effect of severe arthritis in the spine. Spinal fusion can make the spine more stable.
- Repair of damaged disk
Herniated or otherwise damaged disks can bulge out causing pressure on the nerves of the spine. Spinal fusion might be used to stabilize the spine after a damaged disk is removed.
- Correct Spondylosis
Spondylosis is a degenerative arthritis disorder and may result in a loss of normal spinal curvature, structure, and function.
- Correct Spondylolisthesis
This is a condition where one vertebra slips forward relative to the one below.
Patients Ask:
What are the risks of spinal fusion surgery?
Texas Back Institute Responds: In the many years since it was introduced, spinal fusion surgery has been remarkably safe and effective. As with any procedure there are some risks associated with this surgery. Complications include:
Possible spine surgery complications include:
- Infection
- Poor wound healing
- Bleeding
- Blood clots
- Injury to blood vessels or nerves in and around the spine
- Pain at the bone graft site
- Possible bone graft issues
- Return of the symptoms
Spinal Fusion Surgery for Scoliosis Treatment

(Image or photo of x-ray of a patient’s spine with scoliosis)
According to The National Institute of Health, “Scoliosis is a sideways curve of the spine. Everyone has normal curves in the spine, and when looked at from behind, the spine appears straight. However, children and teens with scoliosis have an abnormal S-shaped or C-shaped curve of the spine. The curve can happen on either side of the spine and in different places in the spine.
The NIH notes “scoliosis is estimated to affect 4.5% of the general population. In a nation of approximately 273 million people, this means that over 12 million cases of scoliosis exist, and almost 500 more are diagnosed each day – about 173,000 every year.”
Spine surgeons such as those at Texas Back Institute, diagnose scoliosis by examining a child or teen and taking x-rays. This helps these experts develop a treatment plan, which depends on the location and severity of the curve. Children and teens with milder curves may just need to visit their doctor for regular check-ups. Others may require bracing or surgery.
While there is no definitive cause of scoliosis, wide-ranging research suggests that there is a predisposition for the disease based on families of scoliosis patients. The mother-to-daughter inheritance rate for scoliosis is 1 in 4 or 25%, father-to-daughter is 1 in 10 or 10%, mother-to-son is 1 in 10 or 10% and father-to-son is less than 1 in 20 or 5%.
The spine specialists at Texas Back Institute recognize and treat many different types of scoliosis. Each is evaluated and all are treated differently. These include:
- Idiopathic Scoliosis
This is most often in adolescence (age 10-17). It affects girls much more than boys and is passed down in families. There are also rarer forms that are present before age 10 and this form is not secondary to another condition.
- Neuromuscular Scoliosis
This refers to scoliosis that is secondary to some sort of neuromuscular condition or syndrome. Common ones would include cerebral palsy, myelodysplasia, muscular dystrophy, polio, spinal cord injury, and other conditions. These types of neuromuscular conditions cause muscles to become weak, spastic, or paralyzed. Without full support from the muscles of the back, the spine can develop an abnormal curve as it grows.
Signs of neuromuscular scoliosis often appear early in a child’s life. A parent or the child’s physician will most likely notice your child’s spinal curve through a change in their overall body position or when they start having trouble sitting in a chair. Symptoms may include:
- Leaning or uneven seating posture
- Using arms for seating support
- Uneven shoulder heights
- Head off center from the rest of the body
- Uneven hips or buttocks
- Uneven shoulder blades
- Arms hanging unevenly
- Degenerative Scoliosis
This is an adult-onset form that occurs secondary to the development of degeneration of the spine and its joints. This is most common after the age of 50.
- Congenital Scoliosis
This condition is caused by abnormal development of vertebrae, present at birth. Sometimes vertebrae fail to form normally, or they can fail to segment from each other, leading to an abnormal curvature of the spine. This form can be noticeable at any age in childhood.
For children, treatment options for scoliosis are based on age, gender, and the location and severity of the curve. The curvature is monitored closely and, if necessary, managed with bracing.
While bracing does not cure scoliosis, it may impede the further progression of the curve. If the curve advances despite conservative measures or the measurement of the curve is greater than 40° to 50°, surgical correction is often considered.
With adult scoliosis, treatment planning is generally based on the severity of pain and functional limits. Because of the malalignment of the spine, pain may arise from the facet joints, sacroiliac joints, or from nerve root compression.
The pain from these conditions is managed with physical therapy, medication, facet injections, sacroiliac joint (link to webpage) injections, or epidural steroid injections. If pain persists or physical function is significantly limited, surgery may be considered.
Posterior lumbar fusion (PLF), combined with pedicle screws and rods, is used to realign the spine. Sometimes, anterior lumbar interbody fusion (ALIF) is also done to create a 360° fusion – fusing the front and back portions of the spine.
Scoliosis treatment options include:
o Watchful waiting with serial observation of the curve
o Exercise & physical therapy
o Bracing
o Anti-inflammatory medications
o Surgery
While surgery is always the last option used by the spine specialists at Texas Back Institute, with more challenging or deteriorating conditions such as neuromuscular scoliosis, stabilizing the spine with spinal fusion surgery is used. Using metal rods, hooks, screws, and wires, known as “instrumentation,” the procedure straightens the spine and solidifies the bone so it will no longer curve abnormally.
(insert stock or TBI supplied image of surgery on-going in operating theatre)
For six to 12 months after surgery, the spine fuses in much the same way that a broken bone heals. The child will need to wear a brace during this time. The instrumentation typically remains in the back without causing any problems.
The goal of a spinal fusion surgery for neuromuscular scoliosis is to:
- Stabilize the curve and stop its progression
- Balance the spine and pelvis (in patients who are unable to walk)
- Restore the ability to sit upright (in children who have lost this ability)
- Improve/preserve lung function
Spinal fusion for neuromuscular scoliosis is usually necessary by the time a child reaches adolescence — often sooner than with the milder idiopathic scoliosis. Compared to idiopathic scoliosis, it is usually necessary to fuse a larger portion of the spine to correct neuromuscular scoliosis.
The spine specialists at Texas Back Institute have extensive experience with surgery to correct conditions such as neuromuscular scoliosis. Because there is a potential for a higher rate of complications, safety is paramount throughout the surgical process – from preoperative planning through recovery. Texas Back employs a highly trained team of specialists, all working seamlessly, to mitigate any risk of complications.
Patients Ask:
What is multi-level spinal fusion for low back pain?
Texas Back Institute Responds: In the lower back, a multilevel spinal fusion surgery involves the fusion of two or more motion segments between the first lumbar vertebra, L1, and the first sacral vertebra, S1. The lumbar spine (low back) has 5 mobile spinal levels from L1 to S1, also known as “motion segments.” Fusion of a motion segment involves creating a living “bone bridge” between the two surrounding vertebrae, either behind the disc between the posterior bony elements, through the disc space, or both. This bridge stiffens the spine and stops any motion at the fused motion segment. A bone graft is commonly used to bridge the vertebral bones, which is then replaced by the patient with new native bone.
Spinal Fusion Surgery for Treating Herniated or Bulging Discs
When discs in the spine are damaged to the degree that they must be removed or replaced by an artificial disc, spine surgeons may also recommend spinal fusion surgery.
With every patient, the spine specialists at Texas Back Institute recommend a surgical procedure as the final option. As such, the process of treatment begins with a very conservative approach with suggestions for over-the-counter medications and some behavior (restricting lifting and vigorous activities) modifications.
If this initial plan does not reduce the discomfort or pain from the disc bulge, the next step includes prescription-strength anti-inflammatory and muscle-relaxer medications along with physical therapy to promote strength and range-of-motion in the back or neck, depending on where the herniation is located.
If this step does not alleviate the pain from the damaged disc, the next step would be to get an MRI scan to see where the bulging disc is located, how large it is and to assess its character. After this, some patients require spinal injections, which are a combination of local anesthetics and steroids which are delivered under x-ray guidance into the spinal canal. This will hopefully allow us to reduce the inflammation associated with the bulging disc.
A very small percentage of patients with a bulging or herniated disc will require surgery. This procedure is called a discectomy and is used to decrease the pressure on the nerve by removing the disc fragment in the low back. It is minimally invasive to enable faster healing and recovery time for the patient.
In the neck area of the cervical spine, an approach in front of the spine requires removal of the entire disc and treatment may require replacing the disc or placing a bone graft to replace the space within the vertebral bodies to complete the spinal fusion surgery. Spinal implants are often used in spinal fusion surgery to provide stability and support for the treated area. In the thoracic (mid back) spine, options may include an approach from the back or the side of the chest to remove the fragment away from the spinal cord with or without a fusion.

What is Involved with a 360-Degree Lumbar Fusion?
A 360-degree lumbar fusion is also called an Anterior/Posterior Lumbar fusion. The goal of this procedure is to stop abnormal motion at the location of the involved spinal segments causing pain symptoms.
This is an extremely common method for fusing the lumbar spine. An incision is made in the abdominal area (anterior) and an incision in the lumbar or low back region (posterior). The 360- degree lumbar fusion limits the muscle dissection in the low back compared to other procedures – such as the trans-lumbar interbody fusion procedure -and is less invasive.
Typically, the procedure requires two surgeons to perform – one who is an “anterior access” surgeon and the other who is a spinal surgeon.
In many cases, the spine is closer to the abdomen than it is to the back due to the thickness of the muscle. An access surgeon is responsible for safely maneuvering into the abdomen and exposing the spine. Spine surgeons insert an interbody cage between the vertebra that is filled with synthetic bone graft. This is combined with minimally invasive posterior incisions (usually less than an inch or two) to perform a posterior fusion with screws to hold the spine in place. The 360-degree lumbar fusion success rates are the highest of any spinal fusion.
Minimally invasive spinal fusion techniques offer the benefit of shorter recovery times and hospital stays, with some patients even returning home the same day as their surgery.

What Patients Can Expect with Spinal Fusion Surgery
With any surgical procedure and regardless of the number of times this procedure has been successfully completed, patients are often nervous about what to expect before, during and after the surgery. This is understandable. However, having a “snapshot” of what’s involved in each phase of this surgical process can (hopefully) lead to less anxiety.
Before the spinal fusion surgery
The spine specialists at Texas Back Institute list the following activities, once the decision to have the spinal fusion surgery is made:
- A medical examination, chest X-ray, EKG, and blood work will be completed.
- You may be asked to have a neurological or psychological examination.
- If taking aspirin or anti-inflammatory medications daily, you should stop these medications at least one week before cervical fusion surgery.
- If you take prescription medications or other drugs, including herbals, ask your doctor how soon before cervical fusion surgery you should stop taking these.
- Please do not have anything to eat or drink for 6 to 8 hours before surgery.
- You will check into the hospital the morning of surgery.
- Prior to surgery, you will be asked to sign permits for surgery, anesthesia, blood, and blood products.
During the procedure
- An I.V. (intravenous) line will be initiated. An indwelling catheter may also be ordered by your physician to drain your urine.
- The procedure is done under general anesthesia. This means that you will be asleep for the whole duration of the procedure. A tube to aid your breathing may be inserted through your mouth to help you breathe during the operation.
- If your surgeon is using your own bone for the spinal fusion, he or she will first make an incision on your hip area and gather a ‘bone graft’. If the bone graft is from another person, it will be harvested before your procedure.
- If the affected area is on your lower back, and your surgeon chooses an open procedure, you will be placed in a prone position (lying on your stomach) during the procedure. The surgeon will then create an incision over the region of the affected vertebrae.
- In some cases, spinal fusion may be performed via laparoscopic technique, a less invasive procedure. This technique necessitates several tiny keyhole incisions (rather than one or two large incisions if open surgery), through which the laparoscope and other special surgical instruments are inserted.
- The procedure involves the insertion of the bone graft in between the spaces of two vertebrae. The surgeon may place a plate and screws over the graft to join and hold the vertebral body together until they ‘fuse’ into one bone.
- To complete the procedure, the surgeon will close the incision with stitches.
After the spinal fusion surgery
- The surgeon will contact your family while you are in recovery.
- After going to a hospital room, you will be able to use a PCA pump to get medication for pain control. This machine controls the amount of medication that can be received.
- Staff will usually get you out of bed shortly after surgery.
- The hospital stay is usually 1-2 days.
- A brace or collar is prescribed to restrict bending and promote healing of the fused area.
- Most patients will have some difficulty with swallowing after surgery. This generally improves with time.
- You will be given any needed prescriptions and discharge instructions.
- A set of exercises that you can do at home will be provided.
- You will be able to ride in a car or plane upon leaving the hospital.
- It is important to avoid turning your head and bending your neck excessively.
- After you go home, contact your doctor if you exhibit signs of infection, such as:
- Redness, tenderness or swelling
- Wound drainage
- Shaking chills
- Fever higher than 100.4 F (38 C)
- Physical therapy is usually initiated after the first office visit with your doctor following cervical fusion surgery.
- Recovery from Fusion Surgery varies greatly among patients and is dependent on the extent of the surgery as well as the age and health of the individual.
Bone healing is crucial in the recovery process after spinal fusion surgery, as it ensures the spine fuses effectively and reduces the risk of complications.
Patients Ask:
What is XLIF?
Texas Back Institute Responds: Extreme lateral interbody fusion (XLIF) is a minimally invasive procedure performed through the side of the body to treat spinal disorders and reduce long-term back or leg pain that has not responded to other treatments, such as steroid injections, physical therapy and pain medication. Texas Back Institute surgeons have pioneered minimally invasive surgical procedures because they are completed with very small incisions, resulting in less tissue damage, quicker healing for patients and fewer surgical complications such as infections
What Are the Permanent Restrictions After Spinal Fusion Surgery?
About 8 to12 months after surgery, most patients fully recover and can regain the ability to participate in normal activities. However, spinal fusion patients will never regain the ability to bend, twist, or flex the fused segment. This is because spinal fusion eradicates all motion at the fused segment. This limited mobility is the primary “downside” to having this procedure.
Plus, even when spinal fusion relieves symptoms, it doesn’t prevent future back pain. Most back pain is caused by arthritis and surgery does not cure arthritis.
Other back problems can occur after spinal fusion, and they must be resolved with revision surgery. These include:
- Pseudoarthrosis
This is when the bone graft fails to fuse the vertebrae after spinal fusion. This condition may cause lower back pain but requires imaging tests for diagnosis.
- Recurrent back pain after the procedure
Spinal fusion does not always eliminate back pain. Some patients experience recurrent back pain after this procedure and require additional surgeries
- Adjacent segment disease
Adjacent segment disease, or ASD, is another complication after spinal fusion. It involves the degeneration of the spinal segments neighboring the fused vertebrae. This occurs because the adjacent segments must bear additional impact than usual to accommodate the lack of motion in the fused segment.
- Neurological symptoms like tingling, weakness, numbness, and radiating pain
- Muscle atrophy
Muscle atrophy can affect the back muscles in the area of spinal fusion. This issue commonly affects patients who experience continued pain after spinal fusion. Unfortunately, muscle atrophy can diminish support for the spine..
Having a part of the spine that is less mobile or doesn’t move at all puts more strain on the areas around the fused part. As a result, those areas of the spine might break down faster. Then the spine might need more surgery in the future. It is a good idea to discuss these mobility issues with the experts at Texas Back Institute.
Are You Ready to Improve Your Quality of Life?
Modern medicine, especially when it is combined with the caring doctors and staff at Texas Back Institute, changes patient outcomes. If back pain or injuries are impacting your quality of life, there’s hope and we’re here to help. Click here to set an appointment with the spine experts.
Learn more
Frequently Asked Questions
ACF is a procedure that stabilizes the back by grafting any number of the 2 to 7 vertebrae together. This prevents motion and eases pain. As patients heal, the graft and vertebrae grow together. It is called “anterior cervical fusion” because the procedure is done from the front of the neck. The acronym, PCF, refers to a similar fusion procedure that is done from the back, or posterior, part of the neck.
ALIF or Anterior Lumbar Interbody Fusion, is an approach to spinal fusion surgery where the surgeon accesses and repairs the lower (lumbar) spine from the front (anterior) of the patient’s body. This is usually accomplished through a lower abdominal incision. A TLIF procedure is a Transforaminal Interbody Lumbar Fusion. It treats spinal instability or weakness by permanently uniting bones of the lumbar (lower) spine. TLIF spine surgery is generally less invasive than a posterior spinal fusion (PLIF) with regards to lumbar spinal fusion surgery, but it can sometimes be less effective.
In the many years since it was introduced, spinal fusion surgery has been remarkably safe and effective. As with any procedure there are some risks associated with this surgery. Complications include:
Possible spine surgery complications include:
- Infection
- Poor wound healing
- Bleeding
- Blood clots
- Injury to blood vessels or nerves in and around the spine
- Pain at the bone graft site
- Possible bone graft issues
- Return of the symptoms
In the lower back, a multilevel spinal fusion surgery involves the fusion of two or more motion segments between the first lumbar vertebra, L1, and the first sacral vertebra, S1. The lumbar spine (low back) has 5 mobile spinal levels from L1 to S1, also known as “motion segments.” Fusion of a motion segment involves creating a living “bone bridge” between the two surrounding vertebrae, either behind the disc between the posterior bony elements, through the disc space, or both. This bridge stiffens the spine and stops any motion at the fused motion segment. A bone graft is commonly used to bridge the vertebral bones, which is then replaced by the patient with new native bone.
Extreme lateral interbody fusion (XLIF) is a minimally invasive procedure performed through the side of the body to treat spinal disorders and reduce long-term back or leg pain that has not responded to other treatments, such as steroid injections, physical therapy and pain medication. Texas Back Institute surgeons have pioneered minimally invasive surgical procedures because they are completed with very small incisions, resulting in less tissue damage, quicker healing for patients and fewer surgical complications such as infections
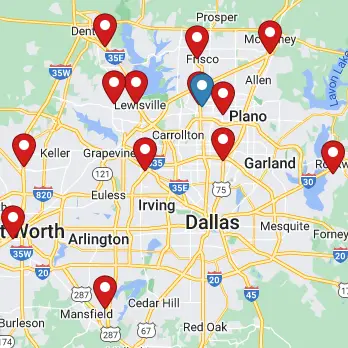
Locations