What is Cervical Fusion?
how we can help
Cervical Fusion Overview
The cervical spine (neck) is comprised of seven stacked bones called vertebrae, labeled C1 through C7. The cervical spine connects to the skull and the upper back at about shoulder level. When viewed from the side, it forms a lordotic curve which is a slight curving toward the front of the body and then back.
Cervical instability is the inability of the cervical spine to maintain its normal placement under physiological loads. Conservative treatment for cervical instability includes physical therapy, bracing, and lifestyle modifications. Minimally invasive treatments include facet joint injections, rhizotomy, and epidural steroid injections. If the pain persists or worsens, surgical intervention such as cervical fusion may be needed to stabilize the spine.
Cervical spinal fusion joins two or more vertebrae in the spinal canal of the cervical spine together to provide greater stability to the neck. It may be necessary:
- After an injury to prevent a bone fracture from causing spinal instability or damage to the spinal cord.
- To address conditions like misalignment of the vertebrae or spinal deformities.
- In combination with decompression surgery to alleviate pressure on the spinal cord and/or spinal nerves caused by degenerative conditions like spinal stenosis, herniated discs, or the effects of osteoarthritis.
- In cases where there is infection or a spinal tumor.
Table of Contents
Treats
Cervical fusion stabilizes the neck by joining vertebrae to treat conditions like:
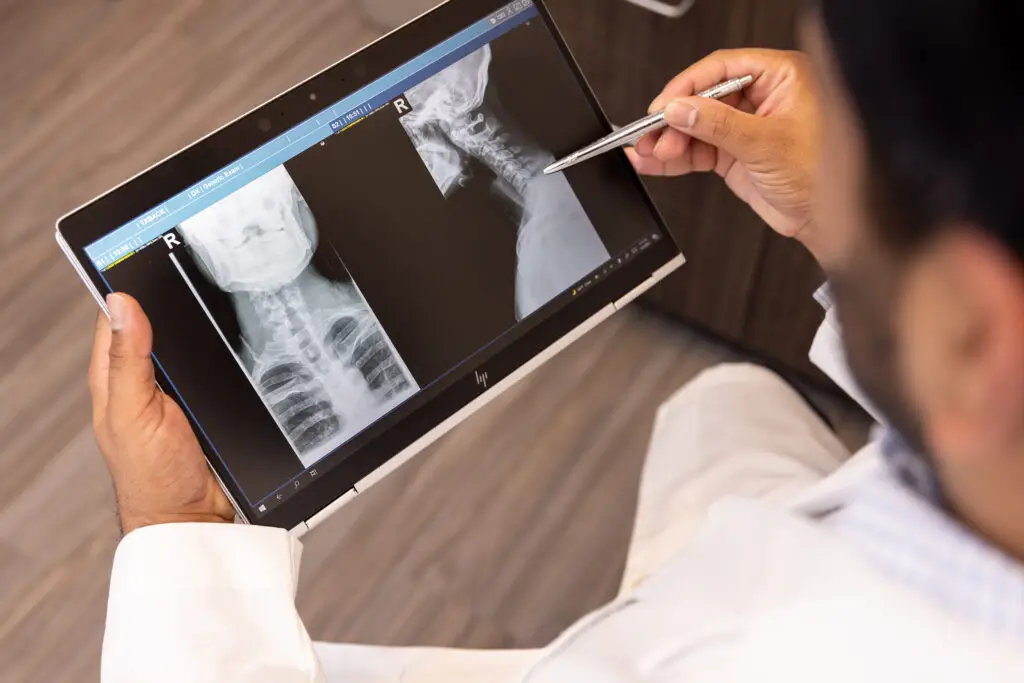
Diagnosing
Cervical spine conditions requiring fusion are diagnosed through a combination of:
Recovery
Recovery from cervical fusion involves:
Patients Ask:
Are there different types of cervical fusion surgical procedures?
Texas Back Institute Responds: Yes, there are several different types of cervical fusion procedures. The differences are based on how the cervical spine is approached during the procedure. Anterior cervical fusion is performed from the front of the body. Posterior cervical fusion is performed from the back of the body. The two most common cervical fusions are the anterior cervical discectomy and fusion (ACDF), and the posterior fusion.
Anterior Cervical Fusion (ACF)
In most cases, patients undergoing Anterior Cervical Fusion procedures have already tried other treatment modalities, including physical therapy, oral pain medications (anti-inflammatories, muscle relaxers, pain killers), and epidural steroid injections. An ACF procedure is done to remove pressure from the nerve roots caused by bone spurs or herniated discs and to stop abnormal movement between two vertebrae.
Once the affected disc has been removed between the vertebrae, a cervical fusion is performed. ACF consists of the surgeon filling the space left by the damaged disc and replacing it with a block of bone. Placing a bone graft between two or more vertebrae causes the vertebrae to grow together, or fuse, during the healing process.
This surgery begins with the anesthesiologist using general anesthesia to put the patient in a sleep-like condition in the operating room. Intraoperative nerve monitoring and x-ray are used to help ensure the safest possible environment. The surgeon and his or her assistants perform the surgery through a small incision on the front of the neck.
The contents of the neck are gently retracted, enabling the front part of the spine to be seen. Important structures, including the trachea, esophagus, and the large blood vessels in the neck are carefully retracted and protected. Once the cervical spine is visualized, the surgeon carefully removes the diseased disc or discs to take the pressure away from the nerves in the spine itself.
Fluoroscopy is used to determine the correct level(s) before the disc material is removed and the fusion graft is inserted. After the disks have been removed, the surgeon reconstructs the spine to restore its height and promote fusion. A surgical plate is then screwed in place over the fusion level.
Anterior Cervical Fusion is performed to treat many spinal conditions, including:

Patients Ask:
Is cervical fusion surgery a high-risk procedure?
Texas Back Institute Responds: ACDF surgery has a high success rate, and patients report that their neck pain and the radiating pain in their arms is resolved after their surgery. Most patients make a full recovery after six months.
As with any surgical procedure, there is a risk of complications. When surgery is done near the spine and spinal cord, these complications can be serious. Complications could involve subsequent pain and impairment and the need for additional surgery. That is why it’s important to discuss all possible complications associated with ACDF surgery with a spine specialist prior to having the operation. At Texas Back Institute, we consider spinal surgery to be the last option in treatment. In fact, many of our patients respond very well to nonsurgical conservative care interventions.
Posterior Cervical Fusion
In a posterior cervical spinal fusion procedure, the bone graft is placed on the back of the vertebrae and often cervical fusion surgery is combined with decompression surgery. A bone graft is placed, and screws or surgical wire is used at the fusion level to provide stability. During the healing process, the vertebrae grow together, creating a solid piece of bone out of the two vertebrae. This type of fusion is rarely used in the cervical spine and generally, only for fractures of the spine.
Posterior cervical fusion may be suggested to straighten the spine or control a spinal deformity, such as cervical kyphosis. This type of spinal deformity can occur when the cervical spine is unstable and begins to bend forward.
Posterior Cervical Fusion is performed to address the following conditions:
- Cervical myelopathy
- Cervical kyphosis
- Cervical spondylolisthesis
- Cervical stenosis
- Failed anterior surgery
- Pseudoarthrosis of anterior fusion attempt
- Ankylosing Spondylitis deformity
- Cervical deformity
Patients Ask:
When will I be able to drive after cervical fusion surgery?
Texas Back Institute Responds: You should avoid driving for several weeks after cervical fusion surgery, as sudden movements could cause pain or damage the surgical site. If a patient is wearing a soft collar to help with comfort, they should refrain from driving until the physician clears them to do so. Collars can limit your ability to turn your neck and body, making it difficult to navigate safely.
What Is Anterior Cervical Discectomy and Fusion (ACDF)?
(insert illustration showing a Anterior cervical fusion)
ACDF is the acronym for Anterior Cervical Discectomy and Fusion, and it has proven to be an effective tool for correcting discs that are herniated.
Healthy discs act as a flexible cushion between vertebrae bones, and this, in turn, allows the neck to bend and rotate. When age-related wear and tear on discs cause herniation or thinning that pinches the nerves, pain and other symptoms can occur.
A discectomy can be performed anywhere along the spine from the neck (cervical) to the low back (lumbar) and a spine surgeon can reach the damaged disc from the front (anterior) of the spine through the throat area. By moving aside the neck muscles, trachea, and esophagus, the disc and bony vertebrae are exposed.
This procedure, where the disc is removed, results in a space or gap between the bony vertebrae. To prevent the vertebrae from collapsing and rubbing together, a “spacer” in the form of a bone graft can be inserted to fill the open disc space. The graft serves as a bridge between the two vertebrae to create a spinal fusion. The bone graft and vertebrae are fixed in place with metal plates and screws.
After this ACDF surgery, the body begins its natural healing process and new bone cells grow around the graft. After 3 to 6 months, the new bone growth and graft should join the two vertebrae and form one solid piece of bone. Instrumentation and fusion work together, like reinforced concrete.
This spinal fusion surgery has proven to stabilize the vertebrae, but patients may notice some range of motion loss. This decrease in mobility will vary according to neck mobility before surgery and the number of levels fused. If only one level is fused, patients may have a similar or even better range of motion than before surgery. If more than two levels are fused, patients may notice limits in turning their head and looking up or down.
Patients Ask:
If my surgeon thinks I am a good candidate, what should I expect?
Texas Back Institute Responds: Cervical arthroplasty is a relatively safe procedure. Surgeons make an incision on the front of the neck, just off of midline – which is relatively pain free since only a small incision is necessary. The trachea and esophagus are moved to the side and blood vessels are moved allowing the diseased disc to be removed using magnification and ensuring that the spinal cord and all the nerves are completely decompressed.
The artificial disc is then implanted using an intraoperative x-ray so that it’s positioned appropriately. The incision is closed with dissolvable sutures. Patients may be given a soft collar to wear to help protect the wound. Some patients stay at the hospital overnight, especially if they are having multiple levels done, but many times patients can go home the same day.
What is Pseudarthrosis?
Pseudarthrosis is a clinical term for bones that do not fuse correctly after injury or surgery. Symptoms may include pain, clicking in the joints, and reduced mobility. However, not everyone with pseudoarthrosis develops symptoms. Pseudoarthrosis can be caused post-operatively by patients who do too much before their vertebrae can fully fuse together.
Other causes of pseudoarthrosis might include:
- Medical Conditions: Ankylosing Spondylitis (AS) can cause vertebral fusion, making the spine less flexible and resulting in a hunched posture. Pseudoarthrosis is a potential complication.
- Congenital Conditions: Although rare, some people are born with pseudoarthrosis – typically located in the clavicle (collarbone) or the tibia (lower leg).
- Surgical Techniques: Some adults that have undergone spinal fusion may develop pseudoarthrosis. Spinal pseudoarthrosis can occur as an adjacent segment disease, which refers to abnormal motion or instability at the level adjacent to a previous spinal fusion.
Symptoms of failed cervical fusion include neck pain that remains or get worse after surgery, muscle tightness with cramping or spasms, pain, weakness, numbness and tingling that radiates from the neck to the arms and hands, and recurrent or residual myelopathy or radiculopathy. Patients typically have a reduced range of motion and mobility when moving their neck.
Dysphagia, or difficulty in swallowing, is a common complication after Anterior Cervical Discectomy and Fusion (ACDF) surgery. Most patients fully recover their ability to swallow within a few days after surgery.

Recovery Process
Recovery from Cervical Fusion Surgery varies greatly among patients and is dependent on the extent of the surgery as well as the age and health of the individual.
To ensure a successful outcome, follow post-operative instructions. Key points to bear in mind during recovery include:
- Activity Restriction: After surgery, patients should limit movement to allow proper healing. Avoid heavy lifting, bending, or twisting. Activity levels will gradually increase with physician approval.
- Neck Brace or Collar: If post-operative care includes wearing a neck brace or collar, follow instructions on when and how to use it.
- Physical Therapy (PT): This should start as instructed by your physician. PT will help restore strength, flexibility, and mobility during the recovery process.
- Incision Care: Keep the incision site clean and dry to prevent infection.
- Diet and Hydration: Eating a balanced diet and staying hydrated promote healing.
- Tobacco Use: Smoking, and even secondhand smoke, can be detrimental to the success of a spinal fusion
- Follow-Up Appointments: Attend all follow-up appointments with your physician to monitor your progress and address any concerns
Benefits of Cervical Fusion Surgery
Cervical spinal stenosis causes pain in the neck area that is the result of constriction to the spinal cord and nerve roots. This is a major concern as cervical stenosis can lead to extreme weakness, swelling and pain. If a person ignores their symptoms, they will worsen over time.
During cervical fusion procedures, surgeons remove painful bone spurs and herniated discs and restore the stability of the cervical spine, promoting better health and preventing further damage. Free from chronic pain, cervical fusion surgery can restore a person’s quality of life.

Knowledge and Experience
As a spine center which has treated patients since 1977, Texas Back Institute has some of the most knowledgeable and experienced spine surgeons in the world. Make an appointment to see one of the world-class spine experts at Texas Back Institute.
Learn more
Frequently Asked Questions
Yes, there are several different types of cervical fusion procedures. The differences are based on how the cervical spine is approached during the procedure. Anterior cervical fusion is performed from the front of the body. Posterior cervical fusion is performed from the back of the body. The two most common cervical fusions are the anterior cervical discectomy and fusion (ACDF), and the posterior fusion.
ACDF surgery has a high success rate, and patients report that their neck pain and the radiating pain in their arms is resolved after their surgery. Most patients make a full recovery after six months.
As with any surgical procedure, there is a risk of complications. When surgery is done near the spine and spinal cord, these complications can be serious. Complications could involve subsequent pain and impairment and the need for additional surgery. That is why it’s important to discuss all possible complications associated with ACDF surgery with a spine specialist prior to having the operation. At Texas Back Institute, we consider spinal surgery to be the last option in treatment. In fact, many of our patients respond very well to nonsurgical conservative care interventions.
You should avoid driving for several weeks after cervical fusion surgery, as sudden movements could cause pain or damage the surgical site. If a patient is wearing a soft collar to help with comfort, they should refrain from driving until the physician clears them to do so. Collars can limit your ability to turn your neck and body, making it difficult to navigate safely.
Locations