Spine Fusion Technology

SPINE FUSION TECHNOLOGY
Over the years, the surgeons at Texas Back Institute have performed thousands of spinal fusion surgeries. Today, we typically perform one of several types of Lumbar Interbody Fusion procedures below. Discuss your case carefully with your doctor and family to determine whether spinal fusion surgery is the right solution for you.
The NuVasive® MAS PLIF procedure is a minimally disruptive approach to traditional back surgery. During a PLIF(Posterior Lumbar Interbody Fusion) procedure, the damaged disc is removed from between two vertebrae in the lower back (the lumbar region). The vertebrae are then fused together to reduce motion. The goals of the procedure are to restore stability in the spine, eliminate pain, and treat common spinal pathologies.
Traditionally, a PLIF is performed by making a midline incision in the patient’s back. The attached muscles are then pulled back and laterally (to the side) to allow sufficient exposure for the surgeon to place pedicle screws for fixation. This often results in postoperative approach-related muscle pain and denervation (loss of nerve supply).
The distinct difference between a traditional “open” PLIF and a MAS PLIF, is the medialized surgical approach. By using a medialized (closer to the spinous process) screw entry point, the MAS PLIF procedure is designed to eliminate the need to retract muscle laterally past the facet joint to the transverse process, therefore requiring a smaller incision than an “open” PLIF. By minimizing the amount of muscle disruption, this procedure is intended to reduce postoperative approach-related muscle pain and enable a faster recovery for the patient.
Patient Benefits
In general, the MAS PLIF procedure results in a shorter recovery and a faster return to normal activities compared to a traditional “open” PLIF procedure.
- Reduced blood loss compared to a traditional PLIF procedure – the MAS PLIF procedure requires a smaller incision and causes less muscle disruption than a traditional PLIF.
- Minimal scarring and postoperative pain – the MAS PLIF procedure avoids excessive lateral dissection/retraction that can cause trauma to and denervation of back muscles.
- Reduced hospital stay – most MAS PLIF patients are discharged from the hospital 1-2 days after surgery.
- Faster return to normal activity – because this procedure is less disruptive than conventional posterior surgery, most patients are able to stand up and walk the evening after surgery.
Potential Risks
Operative and postoperative complications that are known to occur may include early or late infection which may result in the need for additional surgeries; damage to the spinal cord or peripheral nerves, pulmonary emboli; loss of sensory and/or motor function; permanent pain and/or deformity. Rarely, some complications may be fatal. All surgical procedures present risks and complications, and it is important to discuss them with your surgeon prior to surgery. Listening to your surgeon’s guidance, both before and after surgery, will help to encourage the best possible outcome from your procedure.
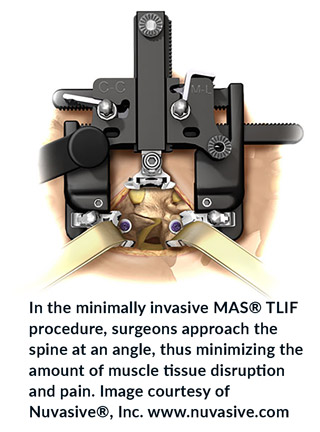
The NuVasive® MAS TLIF procedure is a minimally disruptive approach to traditional back surgery. During a TLIF (Transforaminal Lumbar Interbody Fusion) procedure, the damaged disc is removed from between two vertebrae. The vertebrae are then fused together to reduce motion. The goals of the procedure are to restore stability in the spine, eliminate pain, and treat common spinal pathologies. Traditionally, a TLIF is performed by making an incision in the patient’s back and stripping the posterior muscles to gain access to the spine. This often results in postoperative approach-related pain.
The distinct difference between a traditional “open” TLIF and a MAS TLIF, is the surgical approach. In a MAS TLIF procedure, rather than starting from the center of the back and spreading the muscles outward, the surgical approach involves bluntly splitting the muscles on one side of the back to directly access the surgical site. This enables the surgeon to make a smaller incision with less muscle disruption, resulting in less postoperative pain and a faster recovery for the patient.
Patient Benefits
In general, the MAS TLIF procedure may result in a shorter recovery and a faster return to normal activities compared to a traditional “open” TLIF procedure.
- Reduced blood loss and postoperative pain – the MaXcess® retractor used in the MAS TLIF procedure dilates, rather than cuts, the tissue resulting in less trauma to the affected area.
- Reduced hospital stay – most MAS TLIF patients are discharged from the hospital 1-2 days after surgery.
- Faster return to normal activity – because this procedure is less disruptive than conventional posterior surgery, many patients are able to stand up and walk the evening after surgery.
Potential Risks
Operative and postoperative complications are known to occur may include: early or late infection which may result in the need for additional surgeries; damage to the spinal cord or peripheral nerves, pulmonary emboli; loss of sensory and/or motor function; permanent pain and/or deformity. Rarely, some complications may be fatal. All surgical procedures present risks and complications, and it is important to discuss them with your surgeon prior to surgery. Listening to your surgeon’s guidance both before and after surgery will help promote the best possible outcomes from your procedure.
What is Lateral Access Surgery?
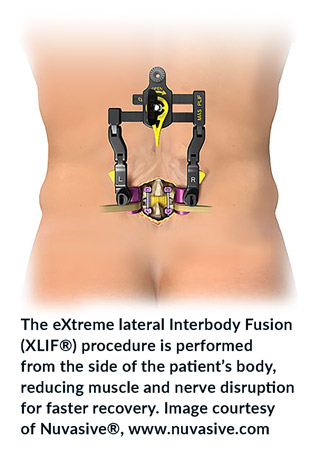
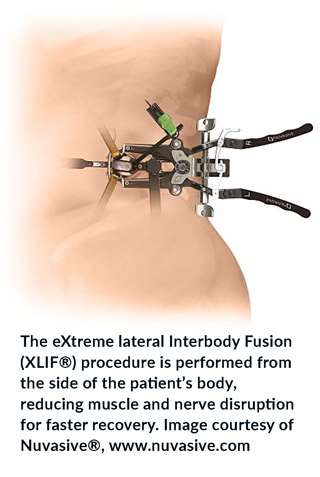
The XLIF® (eXtreme Lateral Interbody Fusion) procedure is a minimally disruptive surgical technique in which the surgeon approaches the spine from the side of the patient’s body, rather than the front or back as in traditional spine surgeries. This side (lateral) approach can reduce the risk of injury to muscles, nerves, and blood vessels. This technique can provide relief to patients who cannot tolerate traditional open back surgery due to increased risks of longer anesthesia time, greater blood loss, longer hospitalization, and slower recovery. XLIF surgery is a less disruptive alternative for patients who have lived with back or leg pain through years of various failed treatments, including steroid injections, physical therapy, and pain medication. The XLIF procedure includes the use of NVM5®, an innovative nerve monitoring system. NVM5 provides surgeons with real-time feedback about relative nerve health, location, and function during surgery, thus reducing the incidence of nerve injury.
Benefits
More than 140 published clinical studies document excellent clinical outcomes following XLIF surgery. For many patients, benefits include:
- Reduced blood loss. A less-invasive procedure allows for less tissue disruption, resulting in reduced blood loss.1-4
- Reduced hospital stay. Patients usually require a stay of one to three days in the hospital, compared to three to six days of immobility and hospitalization typical of traditional open approaches.1-5
- Faster return to normal activity. Many XLIF patients walk the same day they have surgery, as compared to three days later for many traditional lumbar interbody fusion surgeries.5,7
References: 1) Oliveira L, et al. WscJ 2010;1:19-25; 2) Dakwar E, et al. Neurosurg Focus 2010;28(3): E8; 3) Dhall SS, et al. J Neurosurg Spine 2008;9:560-565; 4) Whitecloud TS, et al. J Spinal Disord 2001;14(2):100-103; 5) Deluzio KJ, et al. SAS Journal 2010;4:37-40; 6) Oszgur DM, et al. SAS Journal 2010;4:41-46; 7) Park Y, et al. Spine 2007;32(5):537-543.
What Can You Expect During XLIF Surgery?
Positioning and access. When performing XLIF surgery, your surgeon will approach your spine from the side of your body. You will be positioned on your side on the surgical table. After you have been positioned, an x-ray will be taken to help your doctor precisely locate the operative space. Next, your skin will be marked at the site where the two small incisions will be made. One of the incisions will be on your side—this is the incision from which most of the surgery will be performed. Another incision will be made slightly behind the first, toward your back. Your surgeon will use the latest instrumentation to access the spine in a minimally disruptive manner.
Disc preparation. Disc preparation is the next step. This is done by removing the disc tissue, an action that allows the bones to fuse together. Several x-rays will be taken during this stage to determine whether the preparation is adequate. Once the disc is prepared, the surgeon will then place a stabilizing implant into the space to restore the disc height and help the spine to once again support necessary loads. Once in position, a final x-ray will be taken to confirm correct implant placement.
Fixation. Because further spinal stabilization is necessary, the surgeon will insert additional screws, rods, or plates into the vertebrae.
How Does XLIF Compare to Other Procedures?
Due to advances in medical technology, patients suffering from pain due to degenerative spine conditions now have more options than ever before. Each option has its own set of risks and benefits. Your physician may first attempt to address your problem non-surgically. However, if that does not relieve your pain, he or she might suggest surgery.
Once your physician has recommended spine surgery, the next step is deciding which surgical procedure is appropriate for you. Generally speaking, each procedure is defined by the “approach,” or the way in which the surgeon accesses the spine.
Traditional approaches
Anterior Lumbar Interbody Fusion (ALIF). In this procedure, the spine is approached from the front of the body. This approach spares the back from trauma but requires delicate manipulation of the major blood vessels in front of the spine.
Posterior Lumbar Interbody Fusion (PLIF). This procedure is performed through the middle back, which allows direct access to the area being treated. The downside is that this approach also requires significant disruption to the muscles, bones, and ligaments of the back, which can lead to pain and desensitization after surgery.
Transforaminal Lumbar Interbody Fusion (TLIF). This approach is similar to PLIF; the difference is that only one side of the back is accessed and affected. Like PLIF, significant disruption to the muscles, bones, and ligaments of the back can occur, although these are limited to one side of the back.
Traditionally, both the PLIF and TLIF approaches require significant muscle, bone, and ligament dissection and/or disruption, which can sometimes lead to pain and desensitization of the back muscles after surgery.
Advantages of the lateral approach
The XLIF procedure does not require entry through back muscles, bones, or ligaments, resulting in less postoperative pain. It also allows for complete disc removal and implant insertion, compared with approaches from the back. When compared to ALIF, where the surgeon enters from the front, the XLIF procedure offers the benefit of reducing the risk of vascular injury during the procedure.
Is XLIF Right for You?
Once your physician has concluded that spine surgery is appropriate for you, the best approach for your condition will then be recommended. Some candidates for the XLIF procedure include patients with the following:
Degenerated discs and/or facet joints that cause unnatural motion and pain
- Slippage of one vertebra over another (degenerative spondylolisthesis resulting from advanced degenerative disc disease)
- Change in the normal curvature of the spine (degenerative scoliosis resulting from advanced degenerative disc disease)
Despite its advantages, your physician may decide that the XLIF procedure is not the most appropriate approach for you. The XLIF procedure is not recommended for patients with the following:
Symptoms in the L5-S1 level of the spine
- Certain lumbar deformities
- Severe degenerative spondylolisthesis (significant slip of one vertebra over another)
- Internal abdominal scarring on both left and right sides due to abscess or prior surgery
The materials on this website are for your general educational information only. Information you read on this website cannot replace the relationship that you have with your healthcare professional. You should always talk to your healthcare professional for diagnosis and treatment.
Once your physician has recommended spine surgery, the next step is deciding which surgical procedure is appropriate for you. Generally speaking, each procedure is defined by the “approach,” or the way in which the spine is accessed by the spine surgeon.
Anterior Approaches to the front of the spine:
- Anterior Lumbar Interbody Fusion (ALIF). In this procedure, the spine is approached from the front of the body. This approach spares the back muscles from trauma but requires delicate manipulation of the major blood vessels in front of the spine. It is a generally easier approach for the patient to recover from since no muscles in the abdomen are cut. Patients are typically up walking the same day as their surgery, and depending on the number of levels involved, may be able to go home within 1 or 2 days of their anterior surgery. This is the approach used for lumbar disc replacement and Anterior Lumbar Interbody Fusions.
- Anterior approaches to the cervical spine are used for cervical disc replacement, or for Anterior Cervical Discectomy and Fusion, where damaged discs are removed, the nerves and spinal cord are decompressed, and the cleaned-out disc space is reconstructed.
Posterior Approaches to the back of the spine:
- Posterior cervical and lumbar surgery are most often done when the goal is to remove disc or bone tissue that is pressing on the spinal cord or nerve roots from behind. Nerve root tunnels in the neck can be decompressed from this approach (foraminotomy), often through a Minimally Invasive technique. Lumbar disc herniations are most commonly addressed by a micro-discectomy through a limited posterior approach.
- Posterior Lumbar Interbody Fusion (PLIF). This procedure is performed through the back, usually requiring a midline approach that allows direct access to the area being treated. The downside is that this approach also requires significant disruption to the muscles, bones, and ligaments of the back, which can lead to pain and desensitization after surgery.
- Transforaminal Lumbar Interbody Fusion (TLIF). This approach is similar to PLIF; the difference is that only one side of the back is accessed and affected. Like PLIF, some disruption to the muscles, bones, and ligaments of the back can occur, although these are limited to one side of the back. MIS (Minimally Invasive Surgery) techniques can minimize the amount of trauma to the muscles, and lead to more rapid healing.
Advantages of the lateral approach:
The XLIF procedure does not require entry through back muscles, bones, or ligaments, resulting in less postoperative pain. It also allows for complete disc removal and implant insertion, compared with approaches from the back. When compared to ALIF, where the surgeon enters from the front, the XLIF procedure offers the benefit of reducing the risk of vascular injury during the procedure.
Is XLIF Right for You?
Once your physician has concluded that spine surgery is appropriate for you, the best approach for your condition will then be recommended. Some candidates for the XLIF procedure include patients with the following:
- Degenerated discs and/or facet joints that cause unnatural motion and pain
- Slippage of one vertebra over another (degenerative spondylolisthesis resulting from advanced degenerative disc disease)
- Change in the normal curvature of the spine (degenerative scoliosis resulting from advanced degenerative disc disease)
- Despite its advantages, your physician may decide that the XLIF procedure is not the most appropriate approach for you. The XLIF procedure is not recommended for patients with the following:
- Symptoms at the L5-S1 level of the spine
- Certain lumbar deformities
- Severe degenerative spondylolisthesis (significant slip of one vertebra over another)
- Internal abdominal scarring on both left and right sides due to abscess or prior surgery
The materials on this website are for your general educational information only. Information you read on this website cannot replace the relationship that you have with your healthcare professional. You should always talk to your healthcare professional for diagnosis and treatment.

