Fusion Surgery
 There are multiple ways to fuse a spinal segment. The surgical approach and the exact type of spinal fusion performed depend on the individual’s pain complaints, history of previous surgery, medical health, and spinal structure. The number of levels involved in the fusion depends on the disc levels identified as problematic through diagnostic studies prior to surgery. The particular fusion graft or device to use during surgery will be determined by the surgeon. This decision is based upon individual anatomy, levels of involvement, patient’s medical health, and overall patient safety.
There are multiple ways to fuse a spinal segment. The surgical approach and the exact type of spinal fusion performed depend on the individual’s pain complaints, history of previous surgery, medical health, and spinal structure. The number of levels involved in the fusion depends on the disc levels identified as problematic through diagnostic studies prior to surgery. The particular fusion graft or device to use during surgery will be determined by the surgeon. This decision is based upon individual anatomy, levels of involvement, patient’s medical health, and overall patient safety.
Spinal fusion is designed to reduce movement and immobilize the affected vertebrae making the spine more stable. This technique helps prevent further compression or damage to the spinal cord and nerves by decreasing the added stress that may accelerate with the progression of wear and tear.
The spine is made up of interconnected bones termed the vertebra, which starts from the base of the skull and ends at the tailbone at the lower back. Each bony vertebra sits on top of one another forming the vertebral column. In between each of these vertebral bodies lays a disc cushion called intervertebral discs.
These discs serve as shock absorbers, linking the vertebrae together. These discs also permit the bending and twisting motion of the spine, along with the help of facet joints. Protected within the spinal column is the spinal cord that connects the brain to the rest of the entire body. Spinal nerves arise from this nerve bundle in pairs, one on every side of the vertebra.
Symptoms
- Trauma resulting in a fractured spine or broken vertebra
- Spinal deformities – as a result of scoliosis or kyphosis
- Spondylosis – a degenerative arthritic disorder that may result in a loss of normal spinal curvature, structure, and function
- Weakness or instability of the spine – causing nerve impingement, and pain
- SpondyloIesthesis – a condition wherein one vertebra slides forward relative to the one below
- Herniated or damaged intervertebral discs – also known as ‘slipped disc’, is a condition in which the disc bulges out causing pressure on a spinal nerve
Risks
- Infection
- Bleeding
- Poor wound healing
- Blood clots
- Recurring symptoms
- Pain at the graft site
- Blood vessel or nerve injury
What To Expect
Once you have decided to have Fusion surgery:
- A medical examination, Chest X-ray, EKG, and blood work.
- You may be asked to have a neurological or psychological examination.
- If taking aspirin or anti-inflammatory medications daily, stop these medications at least one week before cervical fusion surgery.
- If you take prescription medications or other drugs, including herbals, ask your doctor how soon before cervical fusion surgery you should stop taking these.
- Do not have anything to eat or drink for 6 to 8 hours before surgery.
- You will check into the hospital the morning of surgery.
- Prior to surgery, you will be asked to sign permits for surgery, anesthesia, blood, and blood products.
Before the procedure:
- An I.V. (intravenous) line will be initiated. An indwelling catheter may also be ordered by your physician to drain your urine.
- The procedure is done under general anesthesia. This means that you will be asleep for the whole duration of the procedure. A tube to aid your breathing may be inserted through your mouth to help you breathe during the operation.
- If your surgeon is using your own bone for the spinal fusion, he or she will first make an incision on your hip area and gather a ‘bone graft’. If the bone graft is from another person, it will be harvested before your procedure.
- If the affected area is on your lower back, and your surgeon chooses an open procedure, you will be placed in a prone position (lying on your stomach) during the procedure. The surgeon will then, create an incision over the region of the affected vertebrae.
- In some cases, a spinal fusion may be performed via laparoscopic technique, a less invasive procedure. This technique necessitates several tiny keyhole incisions (rather than one or two large incisions if open surgery), through which the laparoscope and other special surgical instruments are inserted.
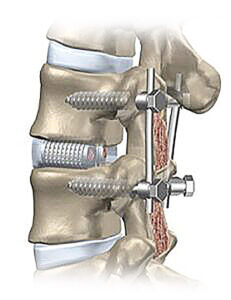
- The procedure involves the insertion of the bone graft in between the spaces of two vertebrae. The surgeon may place a plate and screws over the graft to join and hold the vertebral body together until they ‘fuse’ into one bone.
- To complete the procedure, the surgeon will close the incision with stitches.
You will be in the recovery room from 1 to 1½ hours:
- The surgeon will contact your family while you are in recovery.
- After going to a hospital room, you will be able to use a PCA pump to get medication for pain control. This machine controls the amount of medication that can be received.
- Staff will usually get you out of bed shortly after surgery.
- The hospital stay is usually 1-2 days.
- A brace or collar is prescribed to restrict bending and promote healing of the fused area.
- Most patients will have some difficulty with swallowing after surgery. This generally improves with time.
- You will be given any needed prescriptions and discharge instructions.
- A set of exercises that you can do at home will be provided.
- You will be able to ride in a car or plane upon leaving the hospital.
- It is important to avoid turning your head and bending your neck excessively.
- Physical therapy is usually initiated after the first office visit with your doctor following cervical fusion surgery.
- Recovery from Fusion Surgery varies greatly among patients and is dependent on the extent of the surgery as well as the age and health of the individual.
- Return to work also varies greatly among patients and is related to overall health and the type of work you do. The type of collar used may limit your ability to drive safely for a period of time