Vertebral Fracture Repair
 Watching for progression over time helps determine if a fracture will be stable in the long run. Conditions often treated using Verbal Fracture Repair include:
Watching for progression over time helps determine if a fracture will be stable in the long run. Conditions often treated using Verbal Fracture Repair include:
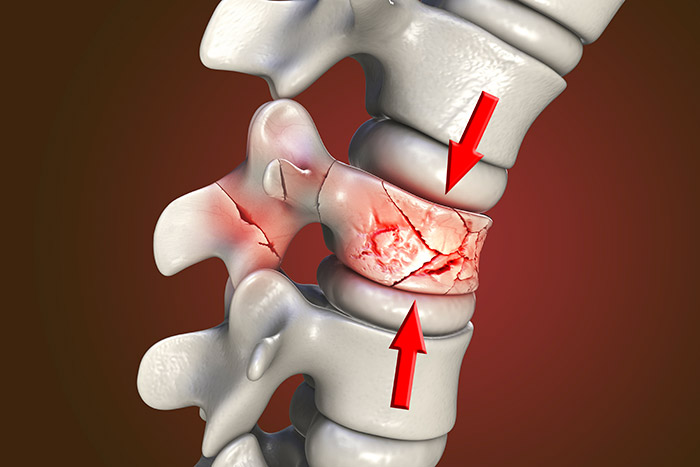
- Vertebral fractures/dislocations/subluxations
- Cervical spine fractures/dislocations/subluxations
- Thoracic spine fractures/dislocations/subluxations
- Lumbar spine fractures/dislocations/subluxations
- Sacral spine fractures/dislocations/subluxations
- Occipetocervical dissociation injuries
- Spinopelvic dissociation injuries
- Spinal cord injuries
- Fractures associated with ankylosing spondylitis
- Fractures associated with osteoporosis
- Fractures associated with cancer/tumors
- Stress fractures of the spine
- Fractures of the pediatric or adult spine
- Fractures of the elderly spine
What to Expect
Once you have decided to have surgery:
- A medical examination.
- Chest X-ray, EKG, and blood work.
- You may be asked to have a neurological or psychological examination.
- If taking aspirin or anti-inflammatory medications daily, stop these medications at least one week before surgery.
- If you take prescription medications or other drugs, including herbals, ask your doctor how soon before surgery you should stop taking these.
- Do not have anything to eat or drink for 6 to 8 hours before surgery.
- You will check into the hospital the morning of surgery.
- Prior to surgery, you will be asked to sign permits for surgery, anesthesia, blood, and blood products.
The procedure usually takes 30 to 45 minutes (longer if more than one level is treated):
- One or two small incisions will be made in your back.
- Fluoroscopy (live X-ray) is used to determine the correct level(s) to be operated on.
- A small tube will be placed through the skin and into the vertebral body and into the center region of the fractured vertebra using x-ray guidance.
- If kyphoplasty is performed, a small balloon-like device is put through the tube and inflated.
- The balloon is then deflated and removed.
- Bone cement will be injected through the tube and into the fractured bone.
- The process may be repeated on the other side of the spine.
You will be in the recovery room from 1 to 1½ hours:
- The surgeon will contact your family while you are in recovery.
- After going to a hospital room, you will be given pain medication if needed.
- Staff will usually get you out of bed shortly after surgery.
- A brace or corset may be prescribed to restrict bending.
- You will be given any needed prescriptions and discharge instructions.
- You will go home the same day or the next day.
- You will be able to ride in a car or plane upon leaving the hospital.
- You will need someone to drive you home.
- Recovery time after vertebral body repair is minimal, although the pain is not always completely eliminated.
Frequently Asked Questions
No. There are many breaks (fractures) that are stable and do not involve injury to nerves or the spinal cord. There is a whole spectrum of severity, and this requires proper medical evaluation.
No. There are many more things that need to be weighed in making that decision. For many patients, surgery in this situation would be futile, and therefore the risk would not be justified.
For others, nonsurgical treatment may have the same expected final outcome, and therefore surgery should be avoided. This is a complex decision that requires evaluation by a spine surgeon.
Generally speaking, either is appropriate. Neurosurgical training involves learning about the treatment of brain and spine conditions, including with surgery.
An orthopedic spine surgeon is an expert in musculoskeletal medicine, including the spine, and generally has done additional specialty training in spine surgery.
As in any specialty, there are surgeons who have particular areas of interest and sub-specialization, with some having more skills and expertise in treating certain conditions. This is probably more important than the neuro vs. ortho division.
Not exactly. It depends on the extent and the location of the fusion. The neck and lower back are the most mobile parts of the spine, so fusions of multiple levels in the neck or lower back result in more permanent stiffness.
The thoracic spine (upper back where the ribs are) does not move as much, so fusion there, even of many segments, does not result in much noticeable loss of motion. Also, a fusion of 1 or 2 levels is of much less consequence than a fusion of more levels.
Not usually. Fixation is generally placed for stability while healing occurs. While it is possible to remove the metal implants in the future, this is generally not done unless some specific reason to remove it develops.
This depends on many factors. The severity of the injury is the main thing that predicts whether improvement is possible, and how much improvement is likely to happen.
The severity of your spinal cord injury is measured by how much loss of function you have initially, as well as the location of the injury in your spine (which vertebral level).
Your medical status and age also affect your ability to improve neurologically. In any given case, this is best predicted by an expert in treating spinal cord injured patients.
It is important to note that surgery may or may not have an effect on this outcome. Surgery can get the pressure off of a compressed spinal cord, or stabilize an unstable spine, but surgery cannot directly repair a damaged spinal cord.
Possibly. The procedure was designed as a minimally invasive procedure done to treat patients who are medically frail/elderly that have broken vertebrae from osteoporosis or cancer/tumors. It is really more like an injection under anesthesia using x-ray guidance.
There is no large incision or wound to heal, there is no real recovery process other than from the sedation/anesthesia, and it is generally a brief procedure, therefore the risks are often acceptable, even in an elderly patient.
The severity of the patient’s medical problems and the severity of the pain, as well as other factors, will need to be considered by your spine specialist in order to decide if it is appropriate to consider this.

