Day 6
We were now starting to fall into a routine. We arrived at the hospital at our “usual” time. Sherri and Rob immediately started setting up the operating room and hunting for yesterday’s tools that we had sent for sterilization. Meanwhile, Izzy, Zvi, Dr. Deo and I rounded on the two surgical patients from the day before. Dr. Deo led us to the surgical wards found in a separate building, much older and smaller than the one we were in. The ward consists of 8-10 private rooms flanking a dim, narrow hallway that opens up on either end to two large common rooms. The perimeter of each large room is lined with cots draped in sheets of all patterns, colours and sizes, leaving a narrow aisle down the centre. The colours are so distracting you could easily miss the patients sprawled on the beds. A stroll down the aisle (which elicits a cascade of curious stares) reveals entire families camped out on mats between and underneath the cots. Children squat and eat from containers of food prepared at home and brought to the hospital. (I later learned that Mbarara does not provide meals to admitted patients, save for malnourished children). It is clear that many have made these cots and mats their surrogate homes. The pathologies in the surgical ward are as eclectic as the bed sheets: limb amputations from motor vehicle accidents and gangrene, bowel obstructions, tuberculosis, breast cancers, malnourished and most disturbing, a young girl with severe burns after acid was thrown on her face. The contrast between this dilapidated surgical ward and the pristine operating theatres of the new building was astonishing.
The women’s room in the surgical ward
Families make the surgical ward their temporary home
After a quick visit with Muhamoud, our patient from yesterday afternoon, we left the surgical ward for the ICU where Amina, our first patient was recovering. We found Amina alert and sitting upright in her bed. Other than some pain around her surgical site, Amina was in fantastic shape. As we left the ICU, Dr. Lieberman smiled and sighed, “It’s a good life.” Our first patient, an 85 year old woman who could barely walk a day before, would live out her remaining years with a grossly improved quality of life.
Back in the operating room, the anesthesia team was prepping our first patient of the day. 28 year-old Naboth had survived a motor vehicle accident only to develop post-traumatic kyphosis (a forward bend of the spine across the collapsed bone).
Dr. Emmanuel, the anesthesiologist, standing in our operating room at Mbarara Regional Referral Hospital
Dr. Lieberman uses the Misonix, an ultrasonic scalpel that only cuts bone, on Naboth
The scene outside the hospital mimicked the drama inside our operating theatre. A heavy thunderstorm (the first rain Mbarara has seen this dry season and therefore a cause for excitement amongst our Ugandan colleagues) was beating down angrily on the hospital. Not surprisingly, Dr. Lieberman had to operate through multiple power outages throughout the day. Thankfully, the ventilator is on an emergency power generator. It was in the midst of this downpour that Dr. Lieberman, Danielle and I held our lunchtime clinic in the open-air corridor outside the operating wing.
Aside from a few more power outages, our second surgery of the day went surprisingly smoothly. This was the second step for Muhamoud, our patient from the previous day. Where his first operation used an anterior (frontal) approach to carve out his necrotic bone tissue, today’s operation would use a posterior (from the back) approach to stabilize and straighten his spine with screws and rods.
At dinner that night, the team discussed some of the mishaps over the last two days and discussed how “old school” is still very important. The ability to adapt to the situation and circumstances at hand, and revert to basic skills is critical to success.
Day 7
Our first operation today was on a beautiful six-year old girl named Prudence. Prudence was born with a cervical rib, an extra rib that sits on top of the first rib and can cause the patient considerable pain. The plan was to remove the articulation (where two bones meet) between the cervical and first ribs. Dr. Lieberman would approach the rib from the left side of Prudence’s neck, very close to some of the most critical nerves and vessels of the upper body. While the team prepped the operating room, I stood and chatted with our little patient. She loves to play football (American soccer) and to watch television cartoons. She used to have four siblings, but her little brother passed away last year at age one from a “hole in his heart.” She was a brave little girl, staring up at the ceiling from her gurney and concentrating hard on hiding any fears about the operation.
Shortly after the surgery began, Dr. Lieberman encountered his first challenge of the day: a branch of the brachial plexus, the meshwork of nerves that provide motor and sensory function to the upper limbs and trunk, traveled directly above the anomalous cervical rib. This would require meticulously careful dissection to avoid leaving Prudence with a neurological problem following surgery. Dr. Lieberman navigated his way around the nerve and the neighbouring external jugular vein, found the cartilage and bone spicule of the articulation and resected without complication. When I went to visit Prudence in the surgical wards that afternoon, she was awake, talking, and most importantly, able to wiggle the fingers of her left hand!
Prudence and her mother in the surgical wards within a few hours of her operation.
After a quick lunchtime clinic, it was on to our second surgery of the day. Rebecca was a 14 year old girl with a congenital hemivertebra (a wedge-shaped vertebra in place of the normal puck shape) and a consequent curve in her spine. The plan was to insert a series of screws and rods into her spine in order to correct the curve, while at the same time resecting the hemivertebra found slightly below the curve. As we prepped Rebecca for the operation, we realized that the operating table wouldn’t accommodate the semicircular arm of our Xray machine. Thinking quickly, Rob checked the operating theatre next door to us and found a woman practically in labour, conveniently perched on a more appropriate operating table. He explained our conundrum and soon enough the birthing mother was being hoisted onto a different bed while Rob snatched the replacement bed out from beneath her and wheeled it back to our OR. To our disappointment, the swapped bed turned out to be a dud too: it could ascend but not descend in height, particularly problematic for an “instrumentation” procedure like Rebecca’s. Finding the next quick solution, Rob brought each member of the surgical team an empty metal instruments box to use as a stepstool. We weren’t in the clear yet. The team flipped Rebecca over onto her belly to expose her spine and as I moved to prep her with an antimicrobial scrub, we realized that our Ugandan colleagues had forgotten to insert her catheter (usually done while the patient lies on his or her back). After a few groans and eye rolls, Rebecca’s catheter was inserted and then finally it was takeoff. Despite three power outages during the surgery (we eventually stopped being phased by the disruption), Rebecca’s surgery proceeded without complication. Our lesson of the day emerged from these mishaps, once again highlighting the importance of thinking quickly on your feet and improving in non-ideal circumstances. It can certainly be a challenge to move quickly and efficiently through patients when the standard procedures you are used to (like prepping and catheterizing a patient) aren’t stream-lined. But then again, life would be boring if we weren’t forced to adapt to new circumstances once in a while!
L-R: Dr. Gorlick, Dr. Joeseph and Dr. Lieberman at the operating table
A nursing student looks on as the surgical team operates on Rebecca.
Almost five hours later, the last stitches went into Rebecca’s back. Dr. Lieberman was visibly exhausted, having just completed his sixth operation in three days (not to mention the seventy-something other patients he’d examined in clinic).
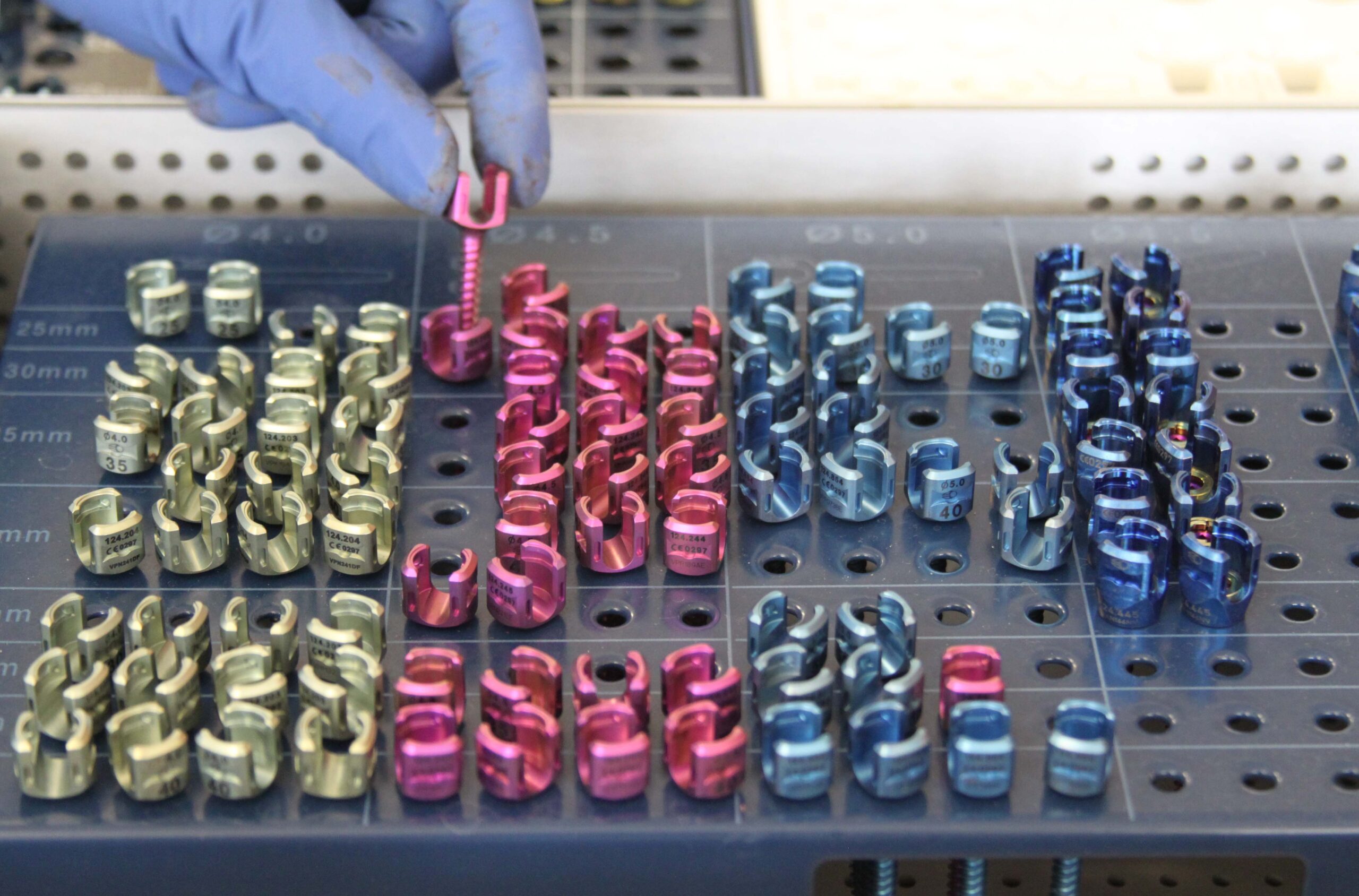
The screws used to stabilize and straighten Rebecca’s spine
After four consecutive dinners at the hotel restaurant, we were desperate for a change in menu. On the recommendation of our driver, we ventured into town for dinner at the Agip Motel restaurant. Despite being a bit skeptical of eating outside our hotel (for reasons of sanitation and stomach bugs), we surveyed the menu and the clientele and took the plunge. An hour, a bottle of wine and several beers later we were satiated and pleased with our decision. As we waited for our dessert to arrive, Dani pulled out her iPhone to show us an app called Heads Up, a charades like game created by Ellen Degeneres and her minions of funny people (so it HAD to be amusing). Sure enough, the team was soon doubled over in hysterics as Rob produced some uncanny impersonations of Sean Connery and Christopher Walken, Dani attempted a bald eagle, and Zvi and I collectively tried to morph into an elk. It was definitely a team bonding evening. We said goodnight to our waitress, Juliana, and promised her we’d return the following night.